Gingival Recession, is there a need for treatment?
Promotional FeaturesPosted by: Dental Design 2nd February 2021

Gingival recession occurs when the gingival margin migrates apical to the cemento-enamel junction (CEJ). With dental implants, the apical shift of the peri-implant mucosa from the crown margin is defined as soft tissue dehiscence.
Common causes of recession around teeth and implants include:
- Toothbrush trauma
- Sub-optimal restoration margins, e.g. Violation of the biologic width
- Unfavourable anatomic factors e.g. tissue morphology and phenotype
- Unfavourable tooth position. e.g. buccally placed teeth
- Unfavourable implant position e.g. outside alveolar envelope
- Orthodontic repositioning outside alveolar envelope or orthodontic relapse
- Periodontal disease
Although most gingival recession is asymptomatic, we have received a significant increase in enquires since the Covid lockdown. The most common complaints relate to tooth sensitivity and aesthetic concerns.
Rationale for treatment:
One study reported that the width of keratinized tissue (KT) is the major predictor for future progression of recession (Chambrone & Tatakis, 2016). Pini Prato 2018 also documented the importance of KT of < 2mm as one of the main contributors for further progression. Other factors include non-carious cervical lesions, smoking and interproximal attachment loss (Pini Prato, Franceschi, Cortellini, & Chambrone, 2018).
The traditional classification for such recessions (Miller’s) has now been updated by a more comprehensive index, advocated by the EFP (European Federation of Periodontology). This classification (Cortellini & Bissada, 2018) attempts to address the multiple causative factors and link them to patient expectations and aids treatment planning.
Surgical root coverage procedures performed to treat root exposure do not always ‘cure’ dentin hypersensitivity. The placement of restorative materials over such defects may therefore still be necessary. In fact, treatment purely aimed at addressing hypersensitivity could be addressed solely with restorative intervention. Currently, composite resin is preferable to glass ionomer cements where higher cosmetic results are desired (Santamaria et al., 2016; Zucchelli et al., 2011).
While preventative restorative measures are effective for many patients, surgical procedures may still be necessary. Root coverage can be achieved by means of a variety of surgical procedures (periodontal plastic surgery). Among the various surgical procedures, the current Cochrane systematic review indicates a greater reduction in recession with subepithelial connective tissue grafts (SCTG) + coronally advanced flap (CAF) when compared to alternative procedures such as CAF with guided tissue regeneration (membranes/acellular dermal matrix or enamel matrix protein) (Chambrone et al., 2018).
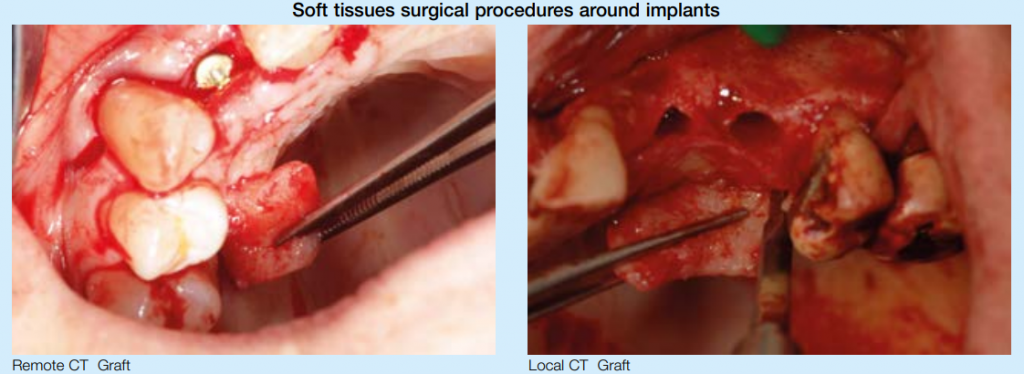
For dental implants, dehiscence is more likely to occur where the soft tissue phenotype is thin and/or if there is an absence of optimal crestal bone. This can be due to sub-optimal implant placement or unsuccessful simultaneous bone augmentation. When an implant is not surrounded by sufficient width of KT, plaque accumulation is more likely as oral hygiene measures may be difficult. Mucositis and peri-implantitis may then ensue. In such situations, soft tissue grafting procedures e.g. FGG or flap manipulation to increase the width of KT is indicated (Roccuzzo, Grasso, & Dalmasso, 2016). Likewise, soft tissue grafting can be used to correct peri-implant recessions to facilitate adequate plaque control and improve aesthetics (Lin & Madi, 2019).

The importance of peri-implant soft tissue thickness in relation to marginal bone resorption has also been investigated. Linkevicius et al 2009 found that thicker tissues favoured marginal bone stability(Linkevicius, Apse, Grybauskas, & Puisys, 2009). It has been hypothesized that the rationale for this phenomenon is due to the reestablishment of the biological width (Berglundh et al., 1991; Cochran, Hermann, Schenk, Higginbottom, & Buser, 1997).Surgical measures to increase soft tissuethickness can be performed prior to implant placement, at time of placement or at the second stage(Thoma et al., 2018).
Conclusion
For both teeth and dental implants, the presence of an adequate width and thickness of soft tissue is crucial to maintain effective plaque control and long-term stability.As clinicians, it is important to educate patients about the risk factors for gingival recession and the likelihood of progression. Understanding the need for adequate soft tissue around implants should be considered in the planning stages to avoid undesirable long-term outcomes.
About the authors

Estela Baz:GDC Number: 208972, Lic Odont. With Special interest in Periodontology. Having received her Periodontics MCinDent from Eastman Dental Institute, Estela now works at the Perio & Implant DRC, limiting her scope of practice to Implants & Periodontics.

Chong Lim:GDC Number: 70007, BDS (National U. of Singapore), MSc in Periodontics (Eastman Dental Inst., UCL), MSc (Distinction) in Dental Implantology (U. of Bristol). Chong heads the Perio & Implant DRC near Richmond Bridge. He is also involved with providing post graduate education for the ITI, Eastman Dental Institute & University of Bristol.








