Dr Kunal Shah explains through a case study how he delivered a high quality restoration using the TBR Z1® dental implant with a zirconia collar.
A 58-year-old male patient presented with a gap in his teeth where the UR5 had been missing for many years. He had been recommended to the practice by another patient. He was fit and healthy with an unremarkable medical history.
Having undergone extensive restorative treatment in the past, the patient was very aware of the different procedures that are currently available to restore teeth. As such, the challenge of this case was to effectively manage the patient – the restorative aspect of treatment was crucial to success, especially as the patient had high expectations of the overall result.
All treatment options were discussed with the patient, including the advantages and disadvantages of each. The patient chose a dental implant as he preferred a fixed solution. The different types of implants available were then discussed with him, including bone- and tissue-level systems. It is important for clinicians to explain treatment options in this level of detail, as patients need to know what each dentist can offer them and/or what else they could access through professional referral. Many patients are also very conscious of what they are putting in their mouth.
As improved aesthetics could be achieved with its zirconia collar design, the patient decided on the Z1® implant system from TBR. This was the most superior yet cost-effective option compared to the alternatives offered. As the Z1® is a tissue-level system, the surgical site does not have to be reopened for the implant to be accessed in order for clinicians to remove the cover screw and replace it with a healing abutment. This saves the patient from having to attend an additional appointment for this, thereby maximising on valuable chairtime.
Furthermore, the Z1® enables clinicians to place the implant in one surgical step, which helps optimise operating room planning and sterilization protocols, making the Z1® much more convenient for patient and practitioner. The versatility of the Z1® also optimises stock management for practices and helps to minimise maintenance treatments for patients. In addition, the Z1® itself was more affordable than the other implant systems that were offered to the patient in this case, providing further cost-saving benefits.
Modern patients are particularly price-conscious, so they need solutions that can achieve the best clinical outcomes whilst meeting their budget.
Treatment planning
Standard treatment planning protocols were followed. This involved taking a CBCT scan to assess the sinus and bone level, as well as provide a 3D view of the proposed surgical site for improved visualisation. A comprehensive assessment confirmed that there was adequate width and height of bone to place an implant. Digital software ensured that the treatment planning process was very precise.
A 4 x 10.5mm tissue-level Z1® implant was planned for, as this solution provides excellent aesthetics and, in this case, did not require a bone grafting procedure prior to surgical placement. Every aspect of treatment was discussed with the patient, before informed consent was obtained for treatment to begin.
Implant placement
Surgery proved to be unremarkable. A delayed implant placement protocol was followed, which involved making a small incision in the gingiva and raising a flap. The surgical site was cleaned and prepared for the implant to be placed successfully and achieve primary anchorage.
The zirconia collar was sunk 1mm into the bone to provide additional stability and boost aesthetics by promoting a good emergence profile. This was accomplished by using the countersink drill in the implant kit. A healing cap was not required due to the transgingival nature of the implant and the design of the zirconia collar, so a cover screw was placed post-surgery.
The surgical site was then assessed, before the patient was sent away with appropriate post-surgery care instructions to take anti-inflammatories and antibiotics to aid the healing process and prevent infection.
Restoration
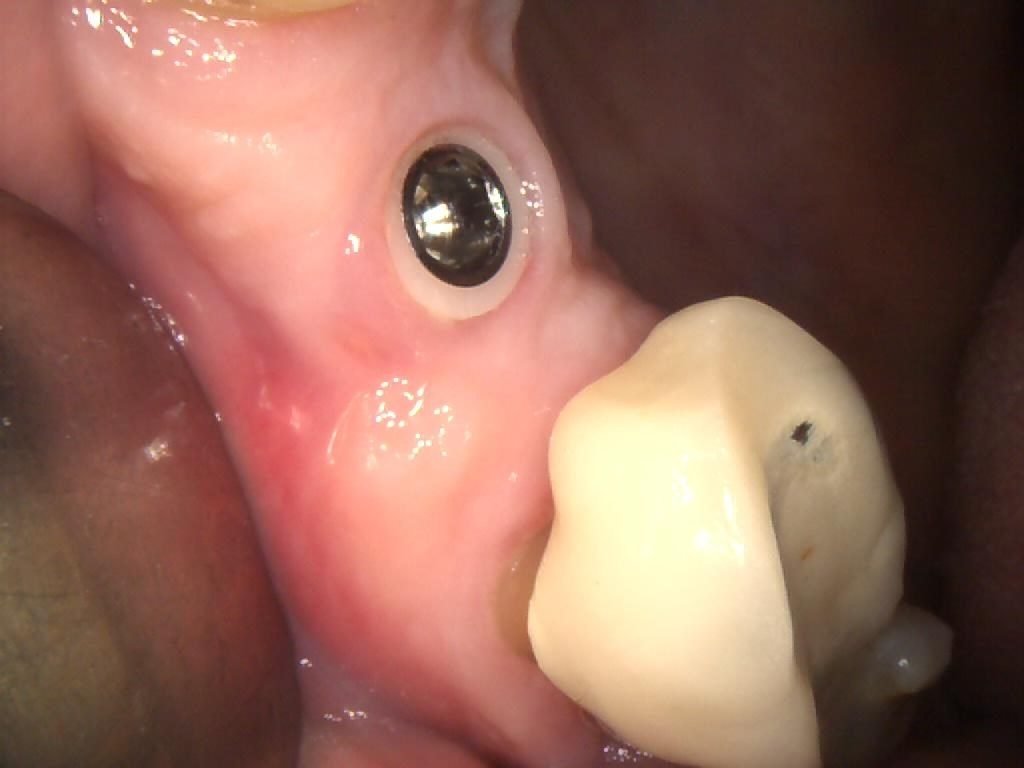
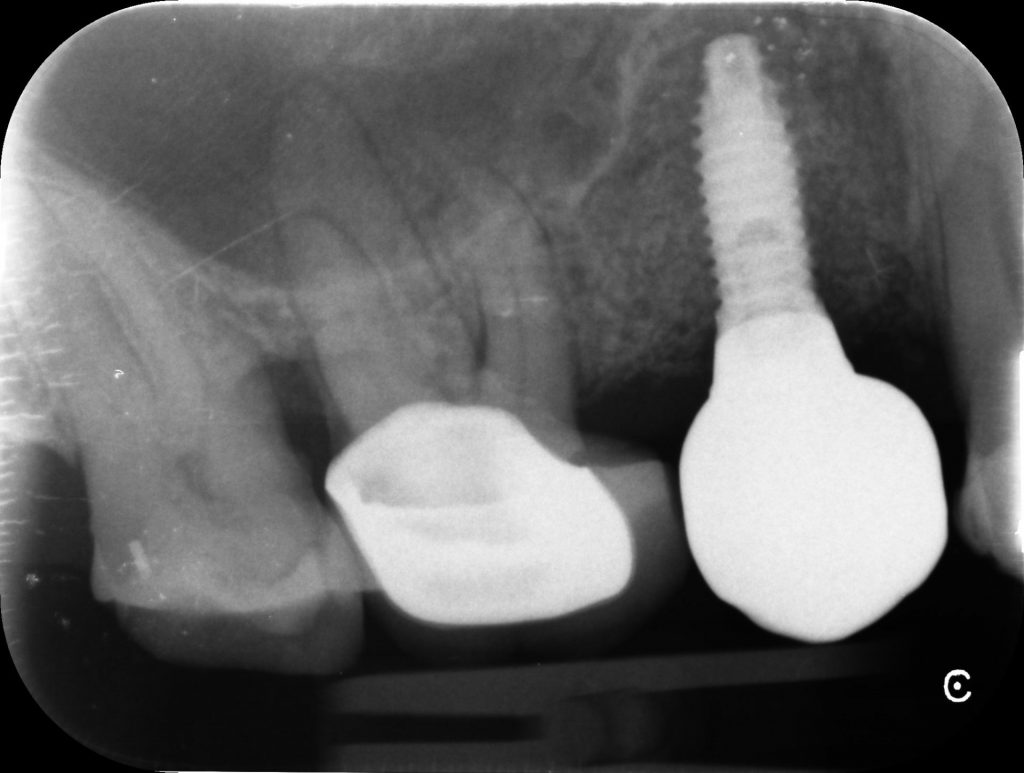
Following 3 months of healing, the implant was evaluated and found to have achieved excellent stability (Figure 1). The soft tissue around the implant was also pink with no inflammation, indicating that it had healed well and was healthy (Figure 2).
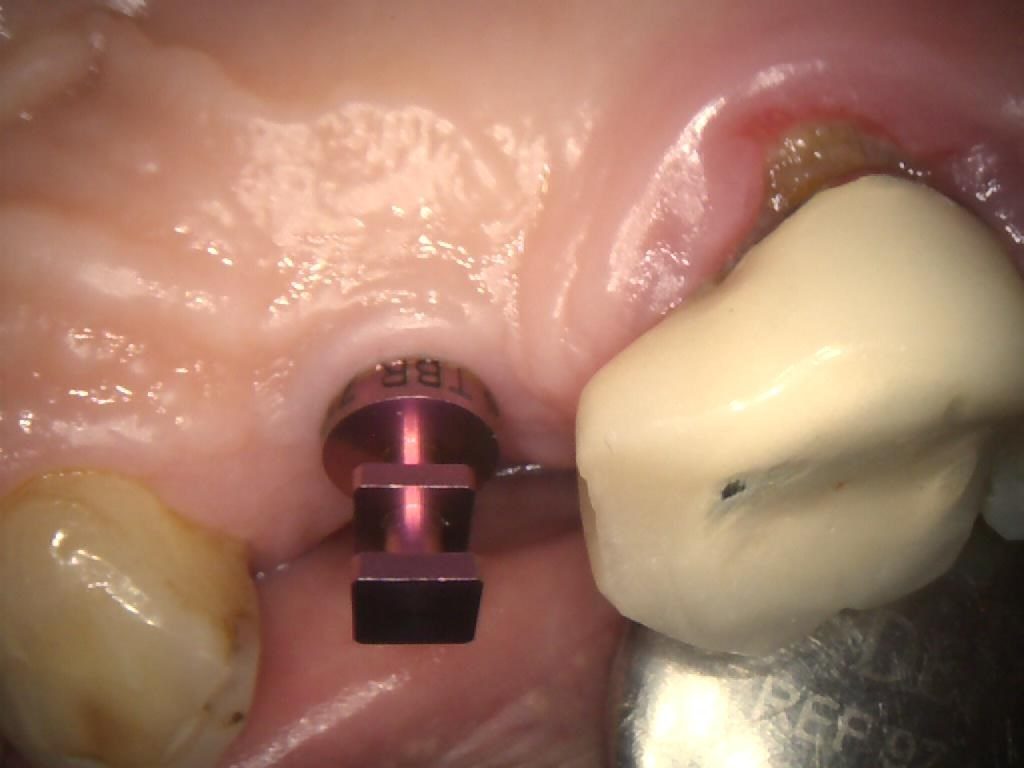
The cover screw was removed (Figures 3, 4 & 5) in order to fit a TBR Swiss Clip impression coping (Figures 6, 7 & 8). This is a very efficient and convenient solution that is quicker than traditional methods of taking an impression, as it simply clips onto the implant. A closed tray impression was taken, alongside a digital scan, which were both sent to the lab to produce a screw-retained E.max crown. The patient chose an implant-retained crown that was a whiter shade than his existing restorations, as he was keen to replace these in the future.
The patient later returned to the practice for placement of the final restoration. The PFM crown was seated (Figures 9, 10 & 11) and the access hole sealed with PTFE tape, before being filled with a temporary dressing (Figure 12). After a week, this was removed and the crown tightened to 25-30Ncm. The screw-access hole was then sealed with PTFE tape and composite.
Clinical and radiographic assessments post-implant restoration show optimal aesthetics and osseointegration (Figure 13). The patient was very happy with the final outcome.
Discussion
In this case, the zirconia collar of the Z1® acted as a healing abutment for the implant to encourage gingival flaring and soft tissue healing for a good gingival profile to develop. This meant that a cover screw could be fitted to the implant and left for 3 months to achieve excellent osseointegration. Simultaneous healing of the hard and soft tissues further emphasised the time-saving benefits that the Z1® provided throughout this case.
The zirconia collar also promoted gingival attachment and served as an antibacterial shield to the crestal bone to prevent iatrogenic inflammation and infection.[i], [ii] This is the only implant system that encourages natural gingival growth, whereas other solutions tend to result in gingival recession over time. Moreover, there are fewer surgical steps involved with placing the Z1®, as you do not need to reopen the surgical site to access the implant for the restorative phase of treatment.
The success of a dental implant is always based on planning treatment correctly. It is also important to offer an implant solution that caters to the needs of the patient. Together, these elements can ensure outstanding results, as was demonstrated in this case. The unique design of the Z1® enabled placement of the implant at tissue-level, thus minimising the number of surgical steps required, which ultimately ensured treatment was less invasive and more convenient for the patient.
Images

Figure 1 – PA Showing UR5 Z1 Infinity 4×10.5m Implant 3 Month Review

Figure 2 – IO Photo Showing UR5 Z1 Infinity Implant with Cover Screw

Figure 3 – IO Photo Showing UR5 Z1 Infinity Implant with Cover Screw Removal

Figure 4 – IO Photo Showing UR5 Z1 Infinity Implant with Cover Screw Removal
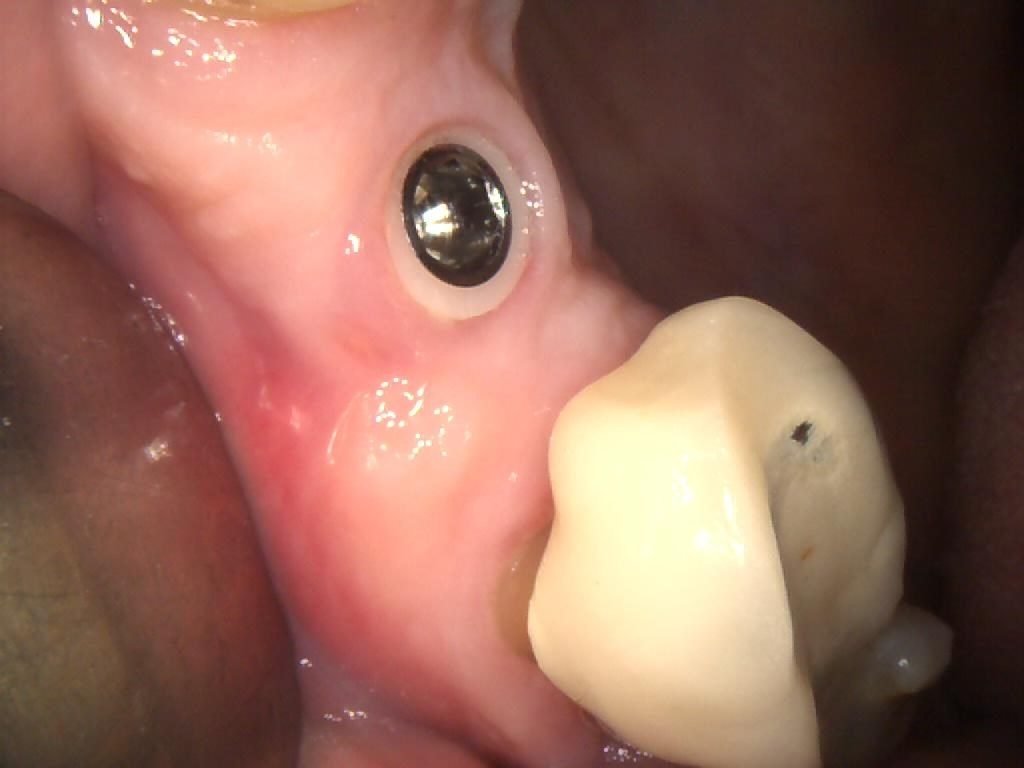
Figure 5 – IO Photo Showing UR5 Z1 Infinity Implant with Cover Screw Removal

Figure 6 – IO Photo Showing UR5 Z1 Infinity Implant with Swiss Clip Impression Coping for Closed Tray Approach

Figure 7 – IO Photo Showing UR5 Z1 Infinity Implant with Swiss Clip Impression Coping for Closed Tray Approach
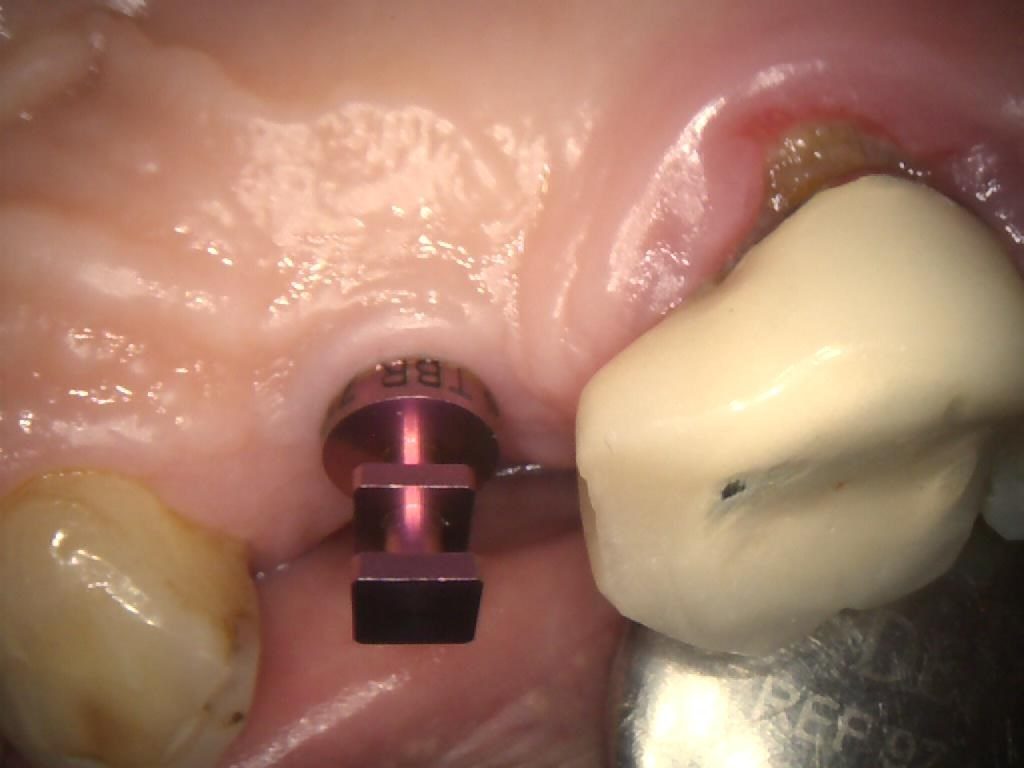
Figure 8 – IO Photo Showing UR5 Z1 Infinity Implant with Swiss Clip Impression Coping for Closed Tray Approach

Figure 9 – IO Photo Showing UR5 Screw Retained Implant Crown Seated

Figure 10 – IO Photo Showing UR5 Screw Retained Implant Crown Seated Buccal View

Figure 11 – IO Photo Showing UR5 Screw Retained Implant Crown Seated Palatal View

Figure 12 – IO Photo Showing UR5 Screw Retained Implant Crown Seated with PTFE tape to protect access hole
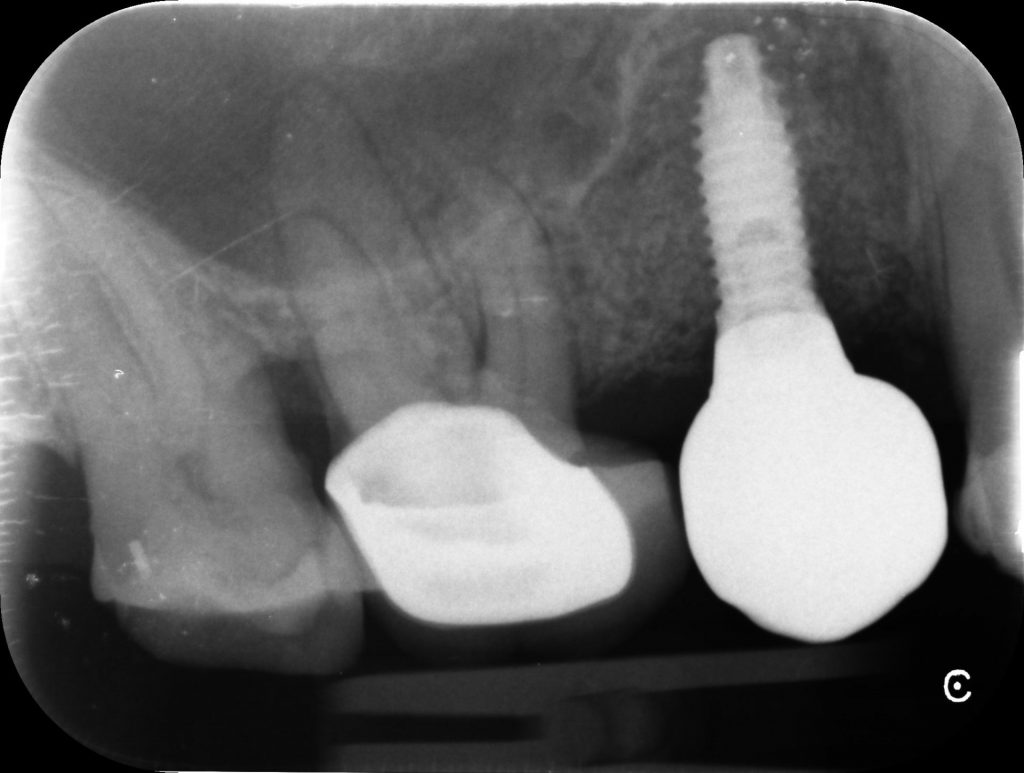
Figure 13 – Post-op PA Showing UR5 Screw Retained Implant Crown Seated
For more information on the Z1® implant, visit tbr.dental, email support@denkauk.com or call 0800 707 6212
Author bio:
Dr Kunal Shah is the Principal of LeoDental in London. He graduated from Birmingham, was selected as a Finalist for ‘Best Young Dentists South’ 2018 at The Dental Awards, and has the accolade for Best Implant and Imaging Clinic – London 2018. Having published several articles in the professional press and lectured internationally, he has a keen interest on the topics of digital dentistry, implantology and restorative dentistry specific to direct resin composites and impression materials. Dr Shah is also a clinical mentor for students on the year-long Post-graduate Implant Course at LeoDental in conjunction with SmileTube.tv.
www.leodental.co.uk
referral@leodental.co.uk
[i] TBR Research Center. (2010) Soft tissue level implant solution: from osseo-integration to perio-integration. Link: https://www.tbr.dental/fr/wp-content/uploads/2018/09/Brochure-ETUDES-2016.pdf. [Last accessed: 16.12.19].
[ii] Yeung, S. C. H. (2008) Biological basis for soft tissue management in implant dentistry. Australian Dental Journal. 53(S1): S39-S42. Link: https://doi.org/10.1111/j.1834-7819.2008.00040.x. [Last accessed: 16.12.19].