Advising patients on diabetes
Featured Products Promotional FeaturesPosted by: Dental Design 31st December 2021
Public Health England (PHE) estimates that over 3.8 million people have diabetes mellitus, with 90% of cases being Type 2 (T2D). The disease can be quite slow to progress, and early symptoms can be difficult for a patient to differentiate from other factors. It is believed that around 1 in 4 people are unaware they have diabetes.[i]Diabetes increases the likelihood of further health complications, of complications occurring during dental treatment, and has been associated with greater COVID-19 mortality.[ii], [iii]
Several demographics are at increased risk of developing T2D. The odds of developing diabetes increase over the course of patients’ lifespans, making older patients much more likely to have the disease (nearly a quarter of over 75s have diabetes, compared to just 9% in middle age). Genetics also play a substantial role with family history, and ethnicity substantially increasing risk (people from south Asian and black ethnic groups are at particular risk). Men are also slightly more likely to develop T2D than women (9.6% vs 7.6%).1
There are certain lifestyle changes that can reduce a patient’s susceptibility to diabetes, and help control their blood sugar if they do develop the condition. The biggest modifiable risk factors are high levels of body fat and physical inactivity, making evidence-based dietary modifications and regular exercise key strategies.[iv] While particularly of benefit to those with pre-diabetes or T2D, these steps tend to promote good health in general, so most patients will benefit from such advice. That said, there are always exceptions. For example, discussing diet with patients with eating disorders can be triggering, and may even provoke a relapse – what may seem like harmless advice to one patient may be inappropriate for another. Care should be taken to tailor support for each patient, instead of simply offering generalisations.
Smoking, including second-hand smoke exposure, increases the risk of developing T2D compared to those with no smoking exposure, by 28%. This association is still observable two to three decades after cessation – though it does improve with time. The risk is dose dependent, so even if patients struggle to quit entirely, they should be encouraged that cutting down on the habit will help somewhat.[v] Patients with children should be made aware that passive smoke exposure puts their children at greater risk of diabetes and other health concerns like heart disease, even if their children never take up the habit themselves.[vi]
Patients may be relieved to know that lifestyle modification is not limited to abstention. Caffeinated and decaffeinated coffee intake reduces the risk of T2D. This effect is quite pronounced, with those drinking three or more cups a day seeing a 25-30% risk reduction.[vii]
 Regular exercise is encouraged for a host of health reasons, but for many patients work and leisure time is dominated by prolonged sitting. Periodically standing and/or walking, even at low intensity confers significant benefits. A study found that standing and walking for five minutes every half hour significantly reduced postprandial glucose, insulin and fatty acid responses in overweight/obese women regarded as at high risk for T2D, compared to participants that sat for prolonged periods. The positive effects on blood glucose and insulin persisted into the following day (where all participants were required to remain seated for 7.5 hours), rather than immediately returning to baseline.[viii]
Regular exercise is encouraged for a host of health reasons, but for many patients work and leisure time is dominated by prolonged sitting. Periodically standing and/or walking, even at low intensity confers significant benefits. A study found that standing and walking for five minutes every half hour significantly reduced postprandial glucose, insulin and fatty acid responses in overweight/obese women regarded as at high risk for T2D, compared to participants that sat for prolonged periods. The positive effects on blood glucose and insulin persisted into the following day (where all participants were required to remain seated for 7.5 hours), rather than immediately returning to baseline.[viii]
We should encourage patients not to think of their health in binary terms. An all or nothing attitude can be discouraging and lead to counterproductive surrendering, or even a nihilistic attitude towards their health. Patients should be validated for making small positive changes, as this will give them a better foundation to make further improvements.
Dental complications associated with T2D include a higher prevalence of caries, xerostomia, oral infections, periodontal disease, salivary gland dysfunction and sensory disorders. The relationship between periodontal disease and diabetes has been established to be bidirectional, with treatment of one improving the other. Edentulism is particularly prevalent among diabetic patients, with over 15% of diabetic patients eventually becoming fully edentulous, and less than 7% retaining all their natural teeth.2
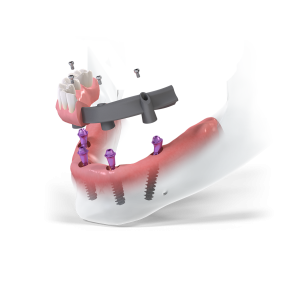
Dental implants are the gold standard in treating edentulism, however, diabetes may raise the risk of complications. Diabetes affects the microvascular system of the gingiva, makes infection more likely, and promotes inflammation, all of which may potentially harm osseointegration and increase the likelihood of peri-implantitis.[ix] Despite this, diabetes is not an absolute contraindication to treatment and success rates are generally very high. Where well-controlled, diabetic status does not appear to impose any additional risk for dental implant therapy.[x]
The Straumann® Pro Arch supports personalised treatment protocols for full-arch restorations. SLActive® surface technology makes it a perfect choice for compromised patients, including those with diabetes or a history of smoking. SLActive® surfaces significantly boost survival rates, and are associated with a very low prevalence of peri-implantitis – just 1.8% over 10 years.[xi]
It is important that patients at risk of, or with, diabetes understand how they can realistically improve their condition. Hopelessness breeds inaction. With good advice and support, diabetes can be managed successfully.
For more information on the Straumann® Pro Arch,
visit https://www.straumann.com/
[i] PHE. 3.8 million people in England now have diabetes. Public Health England. 2016. https://www.gov.uk/government/news/38-million-people-in-england-now-have-diabetes August 26, 2021.
[ii] Nazir M., Al Ghamdi L., Al Kadi M., Al Beajan N., Al Rashoudi L., Al Hussan M. The burden of diabetes, its oral complications and their prevention and management. Open Access Macedonian Journal of Medical Sciences. 2018; 6(8): 1545-1553. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6108795/ August 26, 2021.
[iii] Holman N., Knighton P., Kar P., O’Keefe J., Curley M., Weaver A., Barron E., Bakhai C., Khunti K., Wareham N., Sattar N., Young B., Valabhji J. Type 1 and type 2 diabetes and COVID-19 related mortality in England: a cohort study in people with diabetes. The Lancet Diabetes & Endocrinology. [preprint]. 2020. https://dx.doi.org/10.2139/ssrn.3605226 August 26, 2021.
[iv] Boles A., Kandimalla R., Reddy H. Dynamics of diabetes and obesity: epidemiological perspective. Biochimica et Biophysica (BBA) – Molecular Basis of Disease. 2017; 1863(5): 1026-1036. https://doi.org/10.1016/j.bbadis.2017.01.016 August 26, 2021.
[v] Zhang L., Rimm E., Curhan G., Forman J., Hu F. Association between passive and active smoking and incident type 2 diabetes in women. Diabetes Care. 2011; 34(4): 892-897. https://doi.org/10.2337/dc10-2087 August 26, 2021.
[vi] Diver W., Jacobs E., Gapstur S. Secondhand smoke exposure in childhood and adulthood in relation to adult mortality among never smokers. American Journal of Preventive Medicine. 2018; 55(3): 345-352. https://doi.org/10.1016/j.amepre.2018.05.005 August 26, 2021.
[vii] Kolb H., Martin S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Medicine. 2017; 15: 131. https://doi.org/10.1186/s12916-017-0901-x August 26, 2021.
[viii] Henson J., Davies M., Bodicoat D., Edwardson C., Gill J., Stensel D., Tolfrey K., Dunstan D., Khunti K., Yates T. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: a randomized acute study. Diabetes Care. 2016; 39(1): 130-138. https://doi.org/10.2337/dc15-1240 August 26, 2021.
[ix] Jiang X., Zhu Y., Liu Z., Tian Z., Zhu S. Association between diabetes and dental implant complications: a systematic review and meta-analysis. Acta Odontologica Scandinavica. 2020; 79(1): 9-18. https://doi.org/10.1080/00016357.2020.1761031 August 26, 2021.
[x] Sghaireen M., Alduraywish A., Srivastava K., Shrivastava D., Patil S., Al Habib S., Hamza M., Rahman S., Lynch E., Alam M. Comparative evaluation of dental implant failure among healthy and well-controlled diabetic patients – a 3-year retrospective study. International Journal of Environmental Research and Public Health. 2020; 17: 5253. https://doi.org/10.3390/ijerph17145253 August 27, 2021.
[xi] Buser D., Janner S., Wittneben J., Brägger U., Ramseier C., Salvi G. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clinical Implant Dentistry and Related Research. 2012; 14(6): 839-851. https://doi.org/10.1111/j.1708-8208.2012.00456.x August 27, 2021.









