A 74-year-old retired lady was referred to The Park Dental Practice for the restoration of her missing and failing maxillary dentition with dental implants.
The patient had been suffering from dental phobia for most of her life and had avoided seeing a dentist for regular examination. She only attended when in acute pain and discomfort. This resulted in the loss of all her upper posterior teeth and all her lower molars except the 36 and 46.
Due to a slightly exaggerated gag reflex, the patient could not tolerate a full palate prosthesis. She, however, presented with a ‘horse-shoe’ shaped removable upper acrylic denture, which she reluctantly used for aesthetic reasons only, as it was unstable during chewing.
Her medical history was clear and she was fit and healthy.
The patient’s initial priority was to have her upper jaw restored, with a prosthesis which would be completely stable during function. She also requested the prosthesis to be ‘fixed’ in her mouth on the same day as the remaining failing anterior teeth were extracted. She wanted a low maintenance prosthesis, which would allow for ease of oral hygiene measures.
We discussed the possibility of fixed implant retained bridgework and a removable implant retained denture using Locator attachments. Due to financial constraints, she opted for the latter option. The patient was also aware that if she wanted to ‘upgrade’ to a fixed prosthesis in the future, then that would be possible with Anthogyr Multi-unit abutments.
Assessment
A thorough extra-oral examination, including the patient’s profile and lip support, was carried out (Figure 1).
An intra-oral clinical examination was undertaken, which showed the remaining teeth had drifted and were mobile. The upper alveolar ridges had ample keratinised mucosa with adequate bone width and good bone height (Figure 2).
The lower 46 was compromised and the patient was very reluctant to lose it as it had never caused her any problems. We decided to carry out some root planing of this tooth and keep it under review. The remaining dentition was sound with a healthy periodontal status.
The OPG radiograph confirmed the absence of any pathology in both jaws and the presence of large maxillary sinuses, with inadequate bone volume below them for the placement of dental implants in these regions, without sinus grafts (Figure 3). The patient was very reluctant to undergo any sinus grafting procedures.
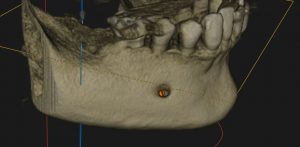
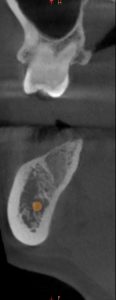
A CBCT scan of the upper jaw was taken to accurately assess the anatomy of the maxilla, the trajectory of the alveolar ridges and to ascertain if immediate implant placement was going to be possible (Figures 4). The scan confirmed adequate bone volume in the anterior maxilla, with good bone height beyond the apices of the failing teeth and intact labial alveolar plates, the density of the trabecular bone was adequate to allow for very good initial primary stability for the immediate placement and loading of the implants.
The CBCT scan also confirmed inadequate bone volume beneath the maxillary sinuses (Figures 5).
A well-fitting immediate partial ‘horse-shoe’ shaped upper acrylic denture was constructed prior to the planned implant surgery. The patient’s consent was obtained during the construction of the denture to ensure that she was happy with the final aesthetic outcome.
The technician had relieved the denture in the anterior alveolar region to allow room for the locator attachments and the metal housings, which would be picked up in the denture, chairside, immediately after implant placement for immediate loading.
implant placement
The CBCT scan was used to plan the immediate placement of implants in the 13 and 24 regions following the extraction of these teeth (Figure 6) and placement in the 14,12 and 22 regions.
Anthogyr Axiom® PX BL (Bone Level) implants – a Straumann Group brand – were placed under intravenous sedation.
One 4 mm diameter/10 mm length implant was placed in the 14 region.
Four 4mm diameter/12mm length implants were placed in the 13, 12, 22 and 24 regions.
All implants were placed in healthy bone using the simple drilling sequence of the Anthogyr implant system. The primary stability achieved was excellent. Locator abutments size 4mm diameter and 3.4mm gingival height were tightened into the implants at a torque of 25Ncm. Platelet rich growth factor (PRGF) was placed into the remaining extraction sockets and the soft tissue sutured (Figure 7).
The locator metal housings were then attached to the Locator abutments (Figure 8) and picked up, in the denture, directly in the mouth with cold-cure acrylic.
Once the acrylic had fully set, securing the metal housings within the removable denture, the denture was removed from the mouth and adjusted (Figure 9).
It was then immediately fitted and secured back onto the Locator attachments (Figure 10). The patient left the surgery with new implant supported teeth.
The locator abutments allow for up to 40-degree angle correction between implants.
Axiom® PX Bone Level® is a very user-friendly implant. The implant surgical kit, and the steps involved during the surgery are straightforward, resulting in minimum trauma to the bone and osteotomy site. The implants afford excellent primary stability, due to the thread design, even in soft bone. The prosthetic kit is also easy to use and sterilise.
Maintenance of the final Prosthesis and Locator abutments
Immediately following surgery, the patient is advised to adhere to a soft diet and not to remove the denture for two weeks, but keep it very clean by brushing and using a Waterpik.
The patient was then reviewed at appropriate intervals to assess healing and an OPG radiograph taken as a baseline record (Figures 11,12,13).
The patient was very pleased with the final aesthetic result, which improved her confidence when talking to people. She was once again able to enjoy chewing food without discomfort (Figures 14,15).
Images

1. pre-op

2. pre-op

3. pre-op OPG

4. extraction

5. immediate loading

6. immediate placement – locators

7. 3 weeks healing

8. 12 weeks healing

9. final 1

10. final 2

11. locator attachment in overdenture

12. post-op OPG
Author bio
Dr Waseem Noordin MSc ImpDent (Lond), BDS, DipImpDent RCS (Eng) (Adv cert), LDS RCS (Eng), MFGDP (UK).
Dr Waseem Noordin is a faculty member of Practical Implant Dentistry Academy, with over 33 years of experience in all aspects of surgical and restorative implant dentistry. He regularly lectures and runs courses in this field. Waseem provides assistance to colleagues in planning cases and one-to-one mentoring in all aspects of implant treatment.
Dr Noordin is a Fellow of the International College of Dentists. He was a tutor, lecturer, cohort director and examiner of the FGDP Diploma in Implant Dentistry at the Royal College of Surgeons of England for ten years. He was a board member of the FGDP (UK) for nine years and director of the Central London Division.
The Park Dental Practice
166 Whitchurch Lane
Edgware
Middlesex HA8 6QL
Tel: 020 8905 6324
Email: theparkdentalpractice@gmail.com
| Figure | Thumbnail | Description |
| 1 | Profile view | |
| 2 | Intra-oral view of remaining maxillary teeth | |
| 3 | The OPG radiograph confirmed the absence of any pathology in both jaws and presence of large maxillary sinuses | |
| 4 | A CBCT scan of the upper jaw was taken to accurately assess the anatomy, bone volume and trajectory of the alveolar ridges | |
| 5 | Inadequate bone below the maxillary sinuses | |
| 6 | Immediate extraction sockets | |
| 7 | Implants placed and Locator abutments attached | |
| 8 | Metal housing on Locator abutments just before pick-up in the denture | |
| 9 | Metal housing precisely secured in the denture. | |
| 10 | Denture fitted immediately following implant placement. | |
| 11 | Anthogyr Axiom® PX BL (Bone Level) implants in the anterior maxilla | |
| 12 | Following three weeks of undisturbed healing | |
| 13 | Following 12 weeks of complete healing | |
| 14 | Anterior view immediately following implant treatment | |
| 15 | Profile view immediately following implant treatment. The patient was very satisfied with the final result. |





 The Year of the Dental Nurse was all about improving the working environment and the opportunities available to individuals in this role. It sought the opinions and experiences of dental nurses throughout Colosseum Dental UK and used these to develop new benefits specifically for them. Among some of the enhancements made were hundreds of pay rises, the chance to learn new skills with training costs covered and the opportunity to earn more as a result of the advanced capabilities obtained. Longer holiday entitlement was also made available to long-standing dental nurses as a thank you for their continued hard work and dedication to their patients.
The Year of the Dental Nurse was all about improving the working environment and the opportunities available to individuals in this role. It sought the opinions and experiences of dental nurses throughout Colosseum Dental UK and used these to develop new benefits specifically for them. Among some of the enhancements made were hundreds of pay rises, the chance to learn new skills with training costs covered and the opportunity to earn more as a result of the advanced capabilities obtained. Longer holiday entitlement was also made available to long-standing dental nurses as a thank you for their continued hard work and dedication to their patients.  The happiness, professional accomplishment and wellbeing of our people matter greatly to us. We will continue to support our people and show that we care more in all that we do. Charlotte concludes:
The happiness, professional accomplishment and wellbeing of our people matter greatly to us. We will continue to support our people and show that we care more in all that we do. Charlotte concludes:


 Emerging trends
Emerging trends














 Your armamentarium is likely to have a number of products that could have greener alternatives available. Look for items that have recyclable packaging or which have been designed to create less waste – these products will last longer, giving you better value for money and reducing the amount of waste generated at the same time. You should also look at products that can streamline your armamentarium – a single product that can replace four or five others is always going to result in less waste, especially as you won’t have to throw away expired adhesives and cements.
Your armamentarium is likely to have a number of products that could have greener alternatives available. Look for items that have recyclable packaging or which have been designed to create less waste – these products will last longer, giving you better value for money and reducing the amount of waste generated at the same time. You should also look at products that can streamline your armamentarium – a single product that can replace four or five others is always going to result in less waste, especially as you won’t have to throw away expired adhesives and cements.


