A 54-year-old female patient, medically fit and well, was referred to me with a retained root in the upper left first premolar region (UL4). The root was infected and the pre-operative radiograph showed the apex of the root to be possibly involved with the sinus floor. The hopeless prognosis of the tooth meant that it required removal during that appointment.
Following extraction healing was uneventful.
Reconstruction
The patient was seen again 6 weeks later, when a radiograph and CBCT (image of scan section available) were taken. ITI classification (SAC) confirmed this as a complex case for implant reconstruction.
All potential treatment options were discussed with the patient. These included no treatment, with common consequences of bone resorption and potential over eruption of the opposing tooth or drifting of the adjacent teeth. Other treatment solutions were restoration with a bridge or an implant-retained prosthetic – including sinus elevation and bone augmentation – and all the likely advantages, disadvantages and possible complications were deliberated. Following explanations of each procedure, informed consent was obtained from the patient, who elected to proceed with an implant placement with simultaneous open sinus lift.
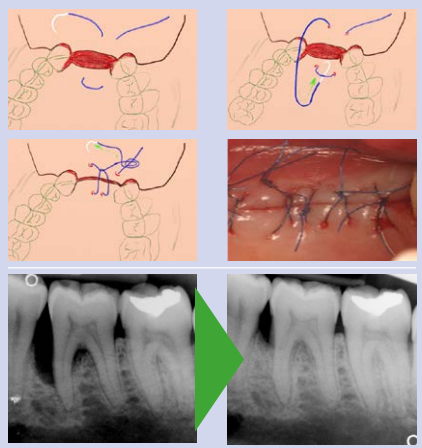
The CBCT was crucial in planning the case. As well as determining adequate mesio-distal space for the planned implant, it allowed assessment of the sinus anatomy and therefore guided both where to prepare the lateral window, and the size of the window that was possible. It allowed measurement from lateral to medial wall within the sinus to further plan the procedure and ensure correct elevation of the membrane and placement of the graft material. This can be seen on the image from the CBCT. The scan also allows visualisation of any blood vessels in the sinus walls and assessment of the thickness of the Schneiderian membrane.
Implant placement
Approximately 3 months after the extraction, the patient returned to the practice for implant placement.
Following local anaesthesia, the patient’s own bone was harvested from the allocated donor site using a bone scraper (Safescraper® Twist, Gietslich). A lateral window was prepared using a diamond bur in a straight surgical handpick with saline irrigation. This was marked with a pencil using measurements taken from the CBCT scan to ensure correct positioning in relation to the sinus floor. The membrane was lifted intact and extended through to the medial wall, again using measurements from the CBCT examination. It can be seen from the preparation that the root of the UL6 was exposed. This is always a potential issue with a sinus lift for a single missing tooth. The post-operative radiograph shows no alteration to the width of the medial root of the tooth, though it will be kept under close radiographic review.
Once the membrane was fully lifted, it was protected during the implant site preparation. The site was prepared for a Straumann® Bone Level Tapered (BLT) implant with Regular Crossfit® (RC) connection and SLActive® surface. The site was underprepared slightly to allow for better primary stability at placement. A tapered implant was selected to further maximise primary stability. The SLActive surface was chosen as clinical trials have suggested that healing periods before prosthetic loading can be reduced using implants with a chemically modified and hydrophilic micro-rough surface.
The harvested autogenous bone was mixed with Giestlich Bio-Oss® granules (0.25mm-1mm) in a 1:4 ratio. Blood collected from the site was used to aid this process. This mix was then packed through the lateral window and condensed to ensure total packing of the lifted region. The Straumann® BLT implant (4.1 x 8mm) was then placed at an initial torque of 30Ncm. A closure cap was placed on the implant to allow complete closure of the flap and protection of the implant and graft during healing.
This mixture of graft materials was used as osteoinductive molecules like bone morphogenetic protein (BMP) and osteogenic cells will enter the augmented site. Bone formation is therefore significantly accelerated as compared to using bone substitutes alone. This allows reduction of healing times, and restorative procedures can be started 3-4 months after the sinus elevation procedure.
The lateral window was checked and then covered with a double layer of Giestlich Bio-gide®. The site was closed carefully with Vicryl 4.0 sutures (Ethicon), ensuring no tension in the soft tissues. The post-operative radiograph demonstrated a good position of the implant and there was good condensation of the graft material.
Upon review 1 week later, the site was healing well and the patient was experiencing no pain or symptoms from the region. The patient was returned to the referring dentist for on-going and routine care with the recommendation that the Implant Stability Quotient (ISQ) is checked at second stage surgery prior to loading.
Taking on cases of this complexity
It is important for all surgeons (and dentists) to continue to follow a Personal Development Plan to allow them to further develop their skills in their chosen area of dentistry. Mentoring and further learning after completion of initial implant training is vital to allow us to recognise cases that may be beyond our current skillset. This is where the ITI SAC classification can play a crucial role in helping clinicians recognise cases that are suitable for their ability or that may need referral. I use the SAC classification in my assessment of every implant patient I see.
I would recommend the ITI to all implant surgeons and restorative dentists as an excellent resource of knowledge and current thinking in implant dentistry and its related fields.
I am a firm believer in continual education and continue to seek out courses that allow me to further develop my skills as a surgeon. Despite having been mentored on sinus elevation techniques and carrying out these procedures for a considerable time, in 2018 I attended The Campbell Academy’s 3-day sinus elevation course and would highly recommend this to anyone looking to carry out sinus elevations.
Images

Figure 1-Pre-operative radiograph

Figure 2-CBCT planning

Figure 3-Preparation of the lateral window

Figure 4-Placement of graft material through lateral window

Figure 5-Implant placement

Figure 6-Membrane placed over graft site

Figure 7-Post-operative radiograph
For more information, please visit www.straumann.com
Author:
Alex Jones is the Principal of Alex Jones Dentistry near Sheffield. He is a very experienced dental implant surgeon, having successfully placed over 2,000 implants. Alex is also currently a member of the ADI and the BACD, as well as a Study Club Director for the ITI.























 Indeed, many dental lab owners have received little, if any, income themselves and whilst wages for some lab staff continue to be covered by the Coronavirus Job Retention Scheme (CJRS), job losses have occurred and may still be inevitable given that the CJRS is coming to an end very soon. There is certainly a great deal of anxiety surrounding cash flow, generating business and managing staff requirements given the uncertainty in relation to the volume of lab work expected moving forward. Many dental technicians fear that they might be made redundant due to these factors, especially as labs are under increasing pressure to either make drastic workforce reductions or close permanently.
Indeed, many dental lab owners have received little, if any, income themselves and whilst wages for some lab staff continue to be covered by the Coronavirus Job Retention Scheme (CJRS), job losses have occurred and may still be inevitable given that the CJRS is coming to an end very soon. There is certainly a great deal of anxiety surrounding cash flow, generating business and managing staff requirements given the uncertainty in relation to the volume of lab work expected moving forward. Many dental technicians fear that they might be made redundant due to these factors, especially as labs are under increasing pressure to either make drastic workforce reductions or close permanently.


