The transition from specialist paediatric dental care to an NHS adult service for children who have suffered a traumatic dental injury (TDI) should be underpinned by an adaptable pathway, according to Emma Morgan, an Academic Clinical Fellow and Dental Core Trainee at Liverpool School of Dentistry and Alder Hey Children’s Hospital.
Her views are based on the feedback of patients who suffered a TDI in childhood and who are referred onwards into an adult service, usually for specialist restorative treatment.
Emma is the 2021 winner of the Max Horsnell Travel Award for her study examining the experiences of young patients as they make the transition from a paediatric to an adult service. She interviewed a group of young people aged 16-21 to get their perspectives.
She explained: “There is no nationally defined transitional care pathway (TCP) and we have limited evidence of what our patients want and need. If the transition is not handled well, it may lead to a failure to engage with adult services and a subsequent gap in care.”
Emma continued: “I got a vast array of opinions from the participants, including a lot of observations about communication. I learned it’s important not to make assumptions about what young people want and need. Young people discussed a number of powerful comments, highlighting the need for involvement of children and young people in research regarding dental trauma.”
Clear communication and involvement of young people in decision making was identified as a vital factor to facilitate a successful experience. The information shared with the patient must be adaptable and driven by them and their needs. For instance, said Emma, “Ideally, our young patients want just the right amount of information to suit them, with both patient and parent involvement. They also want the clinicians in the adult service to be appropriately briefed about their injury and how they feel so they are not forced to discuss potentially distressing experiences with a new clinician.”
Emma hopes that her study entitled The transitional care pathway following traumatic dental injuries: patient perspectives will help to forge a blueprint for a TCP which can be adapted around the country.
She will be presenting her study at the International Association of Dental Research (IADR) meeting in July. Traditionally, the winner of the prize is funded to make a trip to an international meeting. IADR is this year is in Boston, USA. Unluckily for Emma, due to COVID-related travel restrictions, she will not be able to attend in person but the £500 prize money she is being awarded will fund her IADR registration fee.
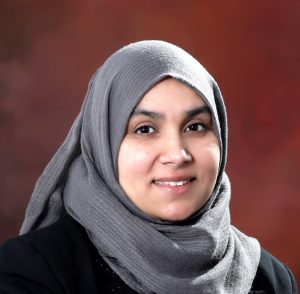
The Student Elective prize in 2021 was won by Nabeela Caratela, an undergraduate at Birmingham Dental School who has been awarded £300 for her abstract examining whether the oral health needs of children in independent schools are being met. Nabeela explained that when she takes diet histories of young patients referred into the Birmingham Dental Hospital, she is aware that children at independent schools appeared to have greater access to refined sugars and was motivated to research whether there is a difference in state and independent school food policies. “I am interested in specialising in paediatric dentistry, to have won this recognition from BSPD is a real privilege.“ More information on Nabeela’s elective will be made available following completion and publication of the study.
BSPD Editor and Chair of the Conference Abstracts and Prizes Committee, Dr Chris Vernazza commented: “Although the pandemic has restricted travel opportunities we had a number of high quality applications to our Max Horsnell Travel Award and Student Elective prizes. It was great to see that UK-based paediatric research will still be promoted globally.”