Everyday life presents many opportunities for accidents to occur. From tripping over your children’s toys to banging your head on an open cupboard, many of us can attest to sustaining some form of personally-inflicted injury from time to time. You’ll likely have encountered many patients who have sustained a dental injury in a similar way. In light of this, it’s important to utilise products that offer the best performance to help restore patients’ teeth to their former glory.
Watch your step
Traumatic dental injuries (TDIs) are often associated with sports or car accidents, violence and occupational incidents. iv [i] TDIs are considered a serious issue in the dentition of children and young adolescents,[ii] who often sustain trauma through falls either at home or at school. Older individuals are also more likely to sustain a dental injury through falls.[iii]
Dental trauma encompasses injuries sustained to the soft and hard tissues of the mouth, such as the teeth and the periodontium.[iv] Such injuries can include luxation, categorised depending on the severity of displacement: concussion, subluxation, extrusive, lateral and intrusive.[v] Luxation injuries are thought to be more common in primary dentition, while crown fractures are often reported in permanent dentition.[vi]Fractures can likewise vary in severity, depending on whether the pulp has been exposed. [vii] Uncomplicated crown fractures include enamel fractures and enamel-dentine fractures, which don’t expose the pulp. More complicated versions include enamel-dentine fractures that do expose the pulp; however, research demonstrates that unless a luxation injury has also been sustained, pulp sensibility tests are usually positive.[viii] In certain situations where the pulp has been exposed, more extensive treatment may be indicated.
TDIs can be sudden and unexpected, and will likely affect the person’s quality of life. While aesthetic concerns may be the initial worry for patients, functional issues can cause complications with mastication and speech.[ix] For patients who delay treatment, whether due to time/financial constraints, a lack of knowledge or dental anxiety, there may be an increased risk of complications within the damaged dentition.[x] This can include pulp necrosis, crown discolouration, root and bone resorption and an infection of the root canal.[xi] In certain situations, seemingly uncomplicated crown fractures can also lead to difficulties, resulting from delayed treatment.ix
Treating the issue
Accidents that cause TDIs can happen at any time, to anyone. Even someone who initially presents with good oral hygiene can suddenly be burdened with additional dental work and care. It’s vital that individuals who sustain a TDI seek dental care as soon as possible. In cases where a non-complicated fracture has occurred, with no involvement of the pulp, treatment can be relatively straightforward with function and aesthetics swiftly restored. In many cases, the fractured piece of tooth can be reattached, which has been recommended by the International Association of Dental Traumatology as the best method for restoring uncomplicated crown fractures in permanent teeth. vii This is, no doubt, preferred by clinicians and patients alike, as the natural tooth can be restored quickly. However, possible complications could include fragment debonding, colour disparity and incomplete fragment rehydration.[xii]
 Alternatively, a composite resin restoration can be placed where reattaching the fragment is not viable. Modern dentistry provides ample restorative solutions that help clinicians achieve outstanding aesthetic and functional results that are natural and long-lasting. When delivering a direct restoration, factors such as colour, translucency, opalescence, shape and surface texture must be taken into account.xi Composite, for example, has become a popular material of choice, due to its longevity, relatively low cost and being easy to repair and replace over time.[xiii] As opposed to direct restorations, research highlights that direct composite restorations have few endodontic complications, and facilitate patient satisfaction/comfort as they can be placed in a single appointment.[xiv] Furthermore, a study found that restorative and biological failures were detected more frequently in teeth restored with a reattached fragment, compare to a direct composite restoration.[xv]
Alternatively, a composite resin restoration can be placed where reattaching the fragment is not viable. Modern dentistry provides ample restorative solutions that help clinicians achieve outstanding aesthetic and functional results that are natural and long-lasting. When delivering a direct restoration, factors such as colour, translucency, opalescence, shape and surface texture must be taken into account.xi Composite, for example, has become a popular material of choice, due to its longevity, relatively low cost and being easy to repair and replace over time.[xiii] As opposed to direct restorations, research highlights that direct composite restorations have few endodontic complications, and facilitate patient satisfaction/comfort as they can be placed in a single appointment.[xiv] Furthermore, a study found that restorative and biological failures were detected more frequently in teeth restored with a reattached fragment, compare to a direct composite restoration.[xv]
A trustworthy product
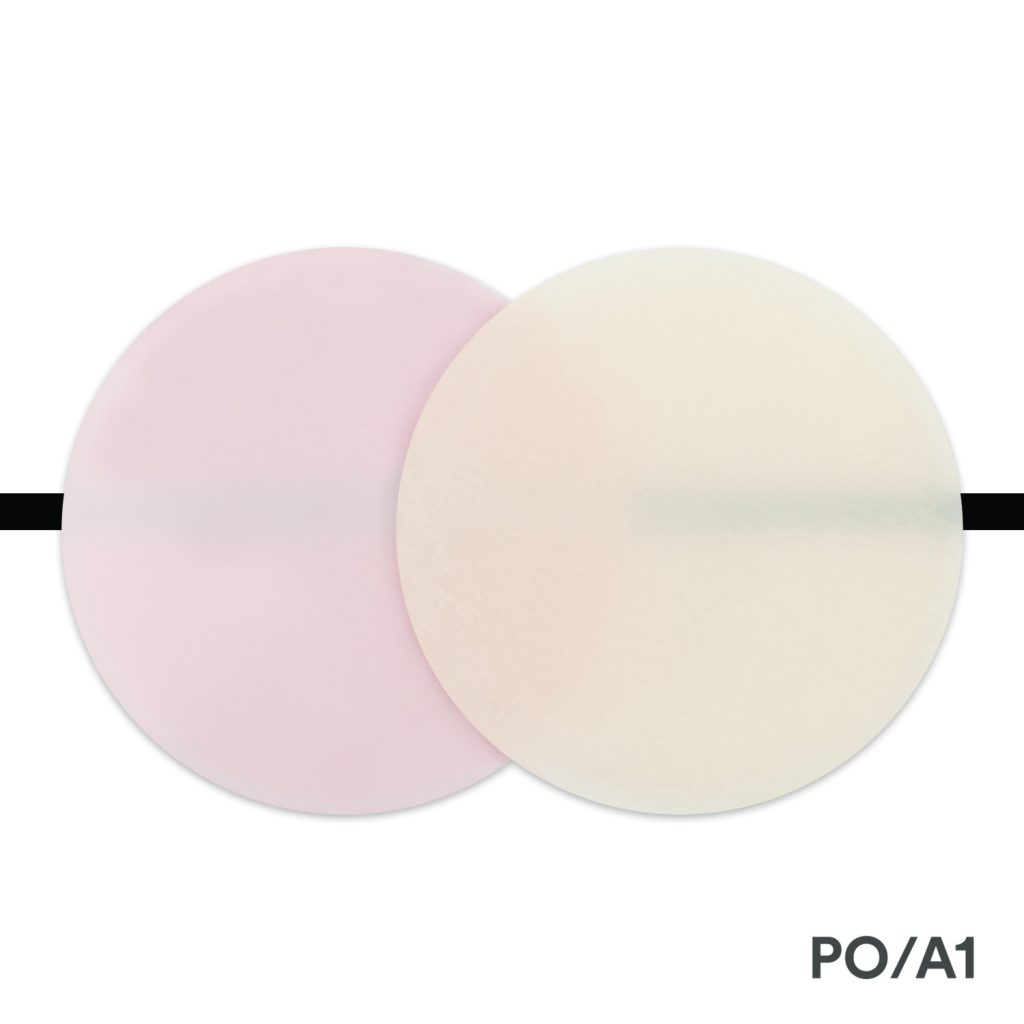
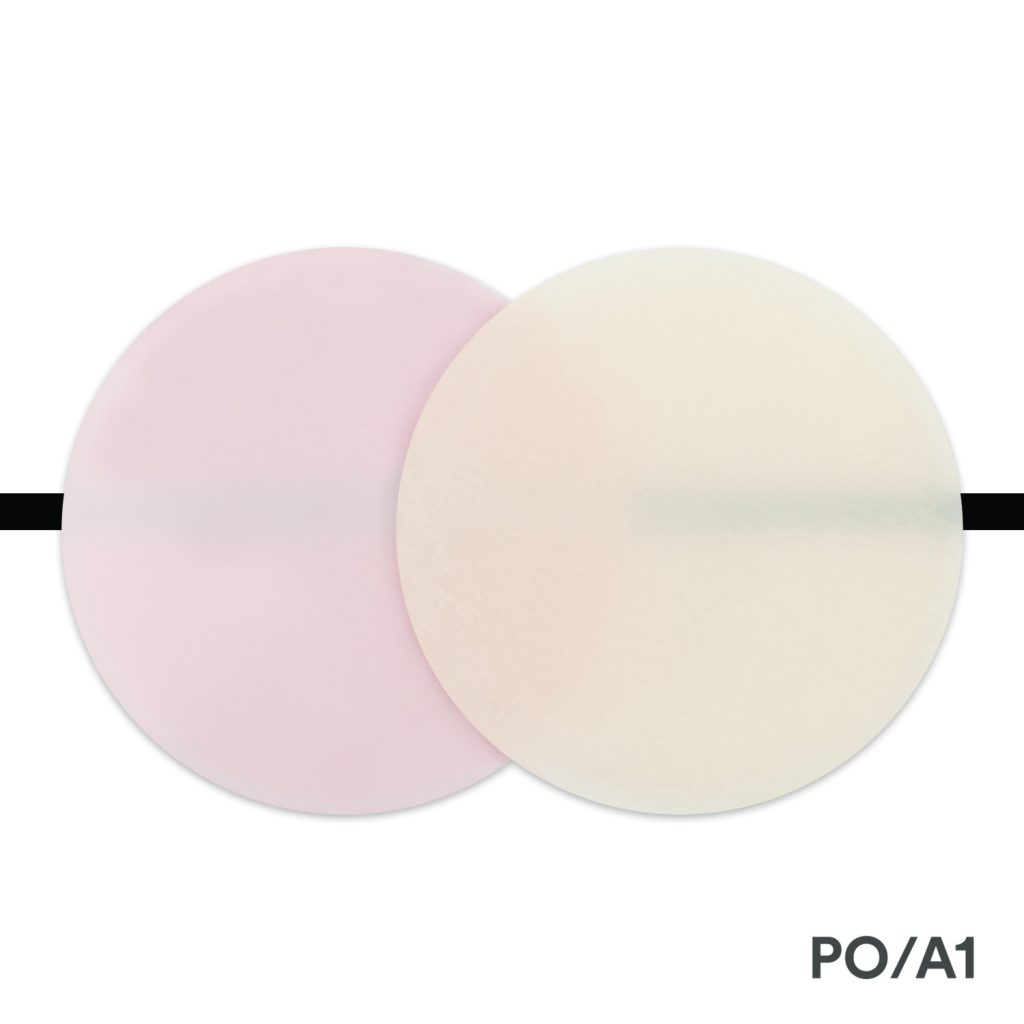
For a simple, easy to use material for direct restorations, the Filtek Universal Restorative from 3M Oral Care should be your product of choice. This solution utilises nanotechnology and fluorescent pigments to deliver a beautifully aesthetic outcome,* with eight designer shades that cover 100% of VITA shades.* Unique features include its high strength, which is suitable for use in stress bearing areas,* and the proprietary low stress monomers help to reduce shrinkage stress.* Filtek Universal Restorative from 3M Oral Care was selected as a top award winner in the 2022 Dental Advisor awards, in the Composite: Universal category!
TDIs can be highly unpleasant experience for patients of all ages, but thankfully, treating them can be straightforward with the right tools, materials and techniques at hand.
For more information, call 0800 626 578 or visit www.3M.co.uk/Dental
3M and Filtek are trademarks of the 3M Company.
*3M Internal data
**Dental Advisor awards 2022: https://www.dentaladvisor.com/evaluations/3m-filtek-universal-restorative/
[i] Kallel, I., Douki, N., Amaidi, S. and Ben Amor, F. (2020). The Incidence of Complications of Dental Trauma and Associated Factors: A Retrospective Study. International Journal of Dentistry, [online] 2020, pp.1–8. Available at: https://www.hindawi.com/journals/ijd/2020/2968174/ [Accessed 17 Nov. 2022].
[ii] Sogi, S., Patidar, D., Patidar, D.C. and Malhotra, A. (2021). Traumatic Dental Injuries in Pediatric Patients: A Retrospective Analysis. International Journal of Clinical Pediatric Dentistry, [online] 14(4), pp.506–511. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8585915/#:~:text=Generally%2C%20children%20are%20likely%20to,to%2014%20years%20of%20age.&text=Accidental%20falls%2C%20road%20traffic%20accidents,dental%20injuries%20in%20children%20worldwide. [Accessed 18 Nov. 2022].
[iii] Patel, J., Wallace, J., Doshi, M., Gadanya, M., Ben Yahya, I., Roseman, J. and Srisilapanan, P. (2021). Oral health for healthy ageing. The Lancet Healthy Longevity, [online] 2(8), pp.e521–e527. Available at: https://www.sciencedirect.com/science/article/pii/S2666756821001422#bib13 [Accessed 17 Nov. 2022].
[iv] Antipovienė, A., Narbutaitė, J. and Virtanen, J.I. (2021). Traumatic Dental Injuries, Treatment and Complications in Children and Adolescents: A Register-Based Study. European Journal of Dentistry. [online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8382465/#:~:text=Dental%20traumas%20are%20injuries%20to,bodily%20injuries%20among%20preschool%20children. [Accessed 16 Nov. 2022].
[v] Goswami, M., Rahman, B. and Singh, S. (2020). Outcomes of luxation injuries to primary teeth-a systematic review. Journal of Oral Biology and Craniofacial Research, [online] 10(2), pp.227–232. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7254462/#:~:text=Luxation%20injuries%20can%20be%20classified,%2C%20extrusion%2C%20intrusion%20and%20avulsion.&text=Avulsion%20or%20ex%2Darticulation%20of,knocked%20out%20of%20the%20socket. [Accessed 16 Nov. 2022].
[vi] Levin, L., Day, P.F., Hicks, L., O’Connell, A., Fouad, A.F., Bourguignon, C. and Abbott, P.V. (2020). International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: General introduction. Dental Traumatology. [online] Available at: https://onlinelibrary.wiley.com/doi/full/10.1111/edt.12574 [Accessed 16 Nov. 2022].
[vii] Mordini, L., Lee, P., Lazaro, R., Biagi, R. and Giannetti, L. (2021b). Sport and Dental Traumatology: Surgical Solutions and Prevention. Dentistry Journal, [online] 9(3), p.33. Available at: https://www.mdpi.com/2304-6767/9/3/33/htm [Accessed 17 Nov. 2022].
[viii] Bourguignon, C., Cohenca, N., Lauridsen, E., Therese Flores, M., O’Connell, A., Day, P., Tsilingaridis, G., Abbott, P.V., Fouad, A.F., Hicks, L., Ove Andreasen, J., Cehreli, Z.C., Harlamb, S., Kahler, B., Oginni, A., Semper, M. and Levin, L. (2020). International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dental Traumatology. [online] Available at: https://onlinelibrary.wiley.com/doi/full/10.1111/edt.12578 [Accessed 17 Nov. 2022].
[ix] Mahmoodi, B., Rahimi-Nedjat, R., Weusmann, J., Azaripour, A., Walter, C. and Willershausen, B. (2015). Traumatic dental injuries in a university hospital: a four-year retrospective study. BMC Oral Health, [online] 15(1). Available at: https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-015-0124-5 [Accessed 17 Nov. 2022].
[x] Chaudhary, S., Singh, H., Gharti, A. and Adhikari, B. (2021). Evaluation of Clinical and Radiographic Findings among Patients with Traumatic Dental Injuries Seeking Delayed Treatment. International Journal of Dentistry, [online] 2021, p.9549508. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8405333/ [Accessed 17 Nov. 2022].
[xi] Lam, R. (2016). Epidemiology and outcomes of traumatic dental injuries: a review of the literature. Australian Dental Journal, [online] 61, pp.4–20. Available at: https://onlinelibrary.wiley.com/doi/10.1111/adj.12395 [Accessed 17 Nov. 2022].
[xii] Lise, D., Vieira, L.C., Araújo, É. and Lopes, G. (2012). Tooth Fragment Reattachment: The Natural Restoration. Operative Dentistry, [online] 37(6), pp.584–590. Available at: https://meridian.allenpress.com/operative-dentistry/article/37/6/584/190603/Tooth-Fragment-Reattachment-The-Natural [Accessed 18 Nov. 2022].
[xiii] Vural, U.K., Kiremitçi, A. and Gökalp, S. (2017). Clinical Performance and Epidemiologic Aspects of Fractured Anterior Teeth Restored with a Composite Resin: A Two-Year Clinical Study. Journal of Prosthodontics, [online] 28(1), pp.e204–e209. Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/jopr.12645 [Accessed 18 Nov. 2022].
[xiv] Apponi, R., Murri dello Diago, A., Colombini, V. and Melis, G. (2021). Direct versus Indirect Techniques to Menage Uncomplicated Crown Fractures of Anterior Teeth Following Dentoalveolar Trauma. Dentistry Journal, [online] 9(2), p.13. Available at: https://www.mdpi.com/2304-6767/9/2/13/htm [Accessed 18 Nov. 2022].
[xv] Haupt, F., Meyerdiercks, C., Kanzow, P. and Wiegand, A. (2022). Survival analysis of fragment reattachments and direct composite restorations in permanent teeth after dental traumatic injuries. Dental Traumatology: Official Publication of International Association for Dental Traumatology. [online] Available at: https://pubmed.ncbi.nlm.nih.gov/36116107/ [Accessed 18 Nov. 2022].









 Alternatively, a composite resin restoration can be placed where reattaching the fragment is not viable. Modern dentistry provides ample restorative solutions that help clinicians achieve outstanding aesthetic and functional results that are natural and long-lasting. When delivering a direct restoration, factors such as colour, translucency, opalescence, shape and surface texture must be taken into account.xi Composite, for example, has become a popular material of choice, due to its longevity, relatively low cost and being easy to repair and replace over time.
Alternatively, a composite resin restoration can be placed where reattaching the fragment is not viable. Modern dentistry provides ample restorative solutions that help clinicians achieve outstanding aesthetic and functional results that are natural and long-lasting. When delivering a direct restoration, factors such as colour, translucency, opalescence, shape and surface texture must be taken into account.xi Composite, for example, has become a popular material of choice, due to its longevity, relatively low cost and being easy to repair and replace over time.