You’ll have heard it before, but it is sometimes easy to forget just how unique every single patient who enters your practice is. After all, each individual leads a completely different life and will have their own habits, quirks and other foibles as well as beliefs and other unique characteristics.
However, these differences can present as challenges in practice, especially if their behaviours impact the state of their dentition. It is partially this that makes restorative dentistry so complex, especially if you have to restore teeth that have become stained over time or through previous treatment.
But what are some of the more challenging aesthetic defects that dentists have to overcome and how can this be achieved?
Masking metal
Although the use of dental amalgam is on the decline in the UK, it still remains a prolific material in the mouths of the general population. The general consensus in dentistry is that the material is going to be phased out (potentially as soon as 2030)[i] but that doesn’t change the fact that a vast number of individuals will already have amalgam in their mouths.
Indeed, statistics suggest that, on average, in 2018 over 90% of the UK adult population had one filling.[ii] This number is likely to have grown throughout the last four years, especially when we consider the impact of the pandemic and the lack of access that people had to dental services during this time.
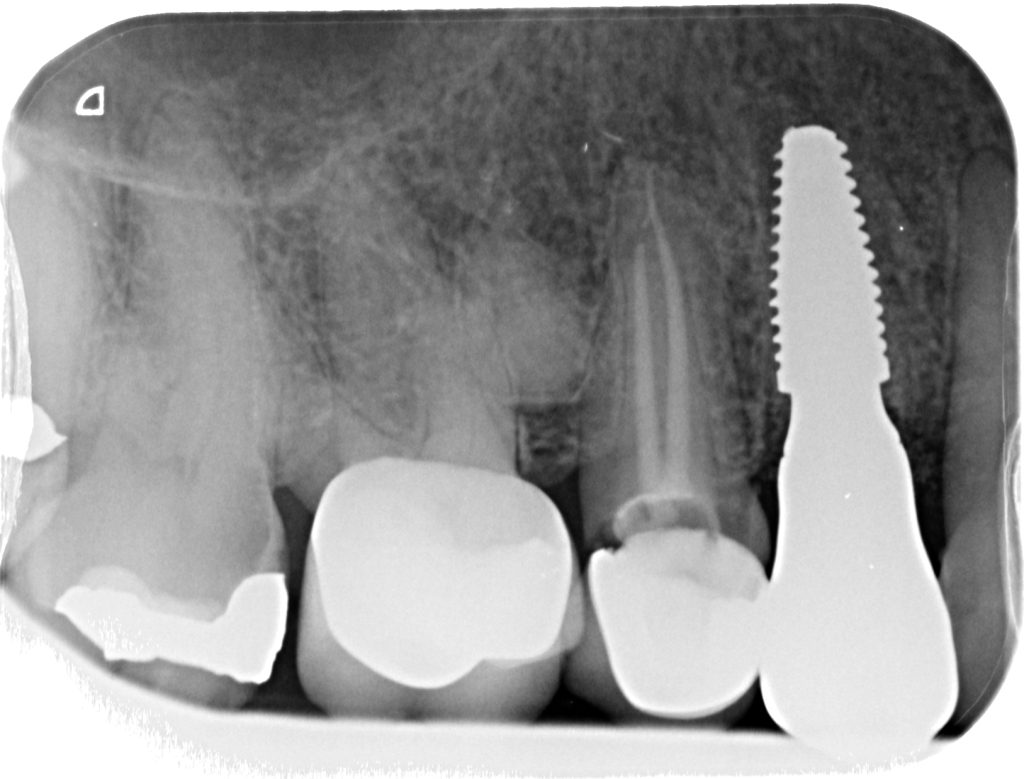
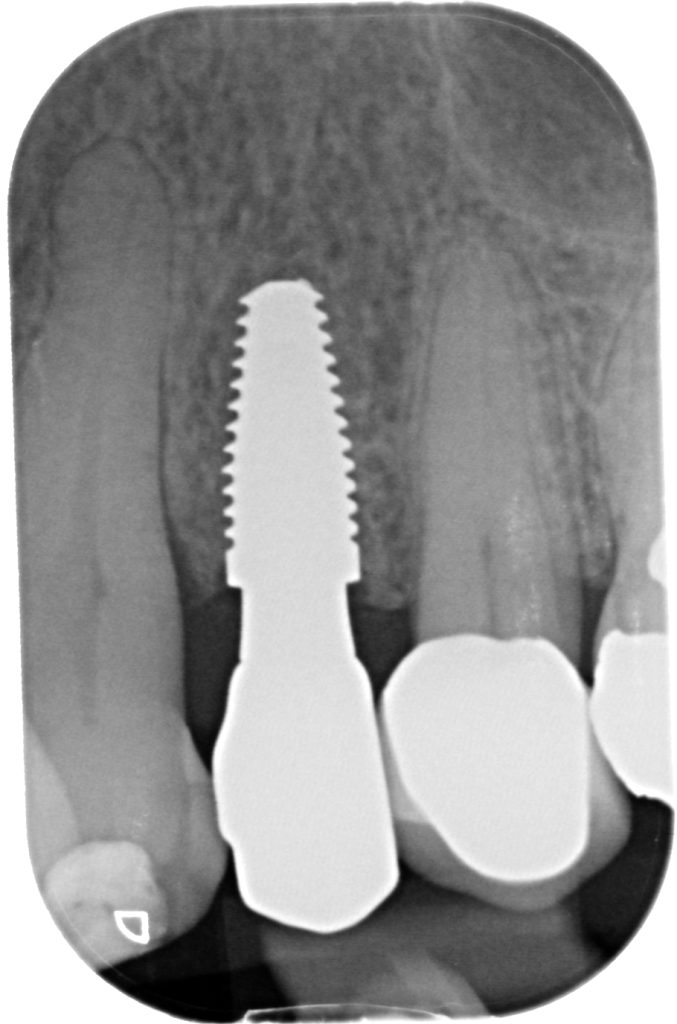
Dental amalgam, though perfectly serviceable, does come with some aesthetic disadvantages. As well as looking unnatural, these types of fillings can also stain the dentition, leading to marks on the surviving natural tooth structure that can be difficult to mask with composite. What makes this a concern for modern dental professionals is that more and more patients are opting to switch their dental amalgam filling for composite alternatives. Though there are no concrete figures indicating just how many patients are making this switch, it’s definitely a priority for people who want to improve their smiles and embrace a more natural look.
As the main ideology behind this behaviour is the quest for a more aesthetic result, patients will want to feel confident that if they do have their fillings redone, their teeth won’t have any residual stains.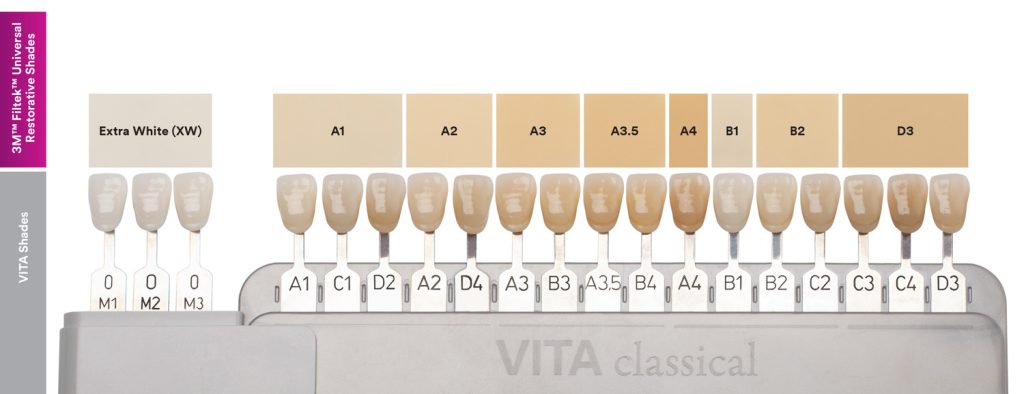
Everyday habits can stain over time
There are many patient behaviours that may lead to tooth-staining. While the vast majority of these are just superficial stains that can easily be solved before restoration, there are certain scenarios where these stains are deeply ingrained and may compromise the aesthetics.
For instance, if a patient chews tobacco or uses recreational drugs – these habits can lead to long-term staining that can be deeply situated within the enamel.
Plus, the development of cavities may also result in stained dentition. As cavities often present as dark grey, black or brown spots, and any dentine that is affected by caries may be discoloured, even after the decay is cut away – these scenarios can provide professionals with challenging cases.
Medications make a difference
Interestingly, there are a few medications that can result in stained dentition. Tetracycline, for instance, has been proven to cause tooth staining and marks that look like discoloured lines forming along the tooth. This phenomenon usually occurs when children are given these antibiotics, which has led to the medicine being restricted for use in younger age groups. However, with it being a popular medication years ago, there are still patients who have tetracycline-stained dentition and will need extra attention when it comes to restorations.[iii]
Everyday adjuncts to oral hygiene including some mouthwashes have also been linked to tooth staining, while certain antihistamines, antipsychotic drugs and antihypertensive medicines have been found to discolour teeth too, creating stains that are difficult to remove.
 Your key to aesthetics
Your key to aesthetics
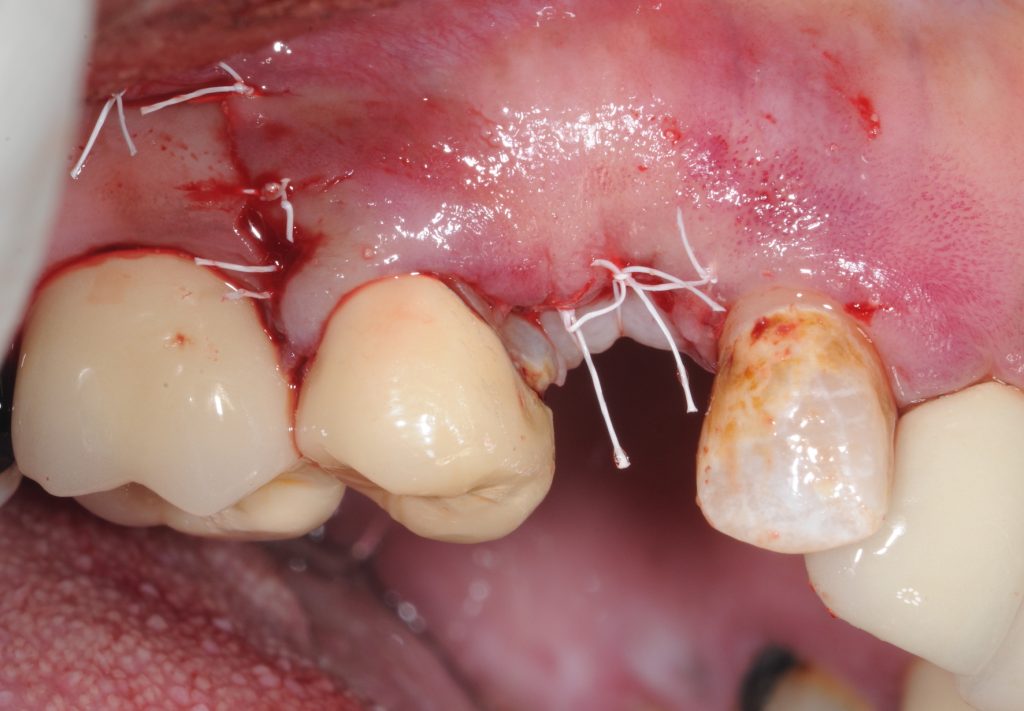
Finding composites that can reliably cover stained dentition isn’t always straightforward. Depending on the opacity and shade of the composite being used, stains can persist and remain visible, leading to poor final aesthetics that will likely impact patient satisfaction.
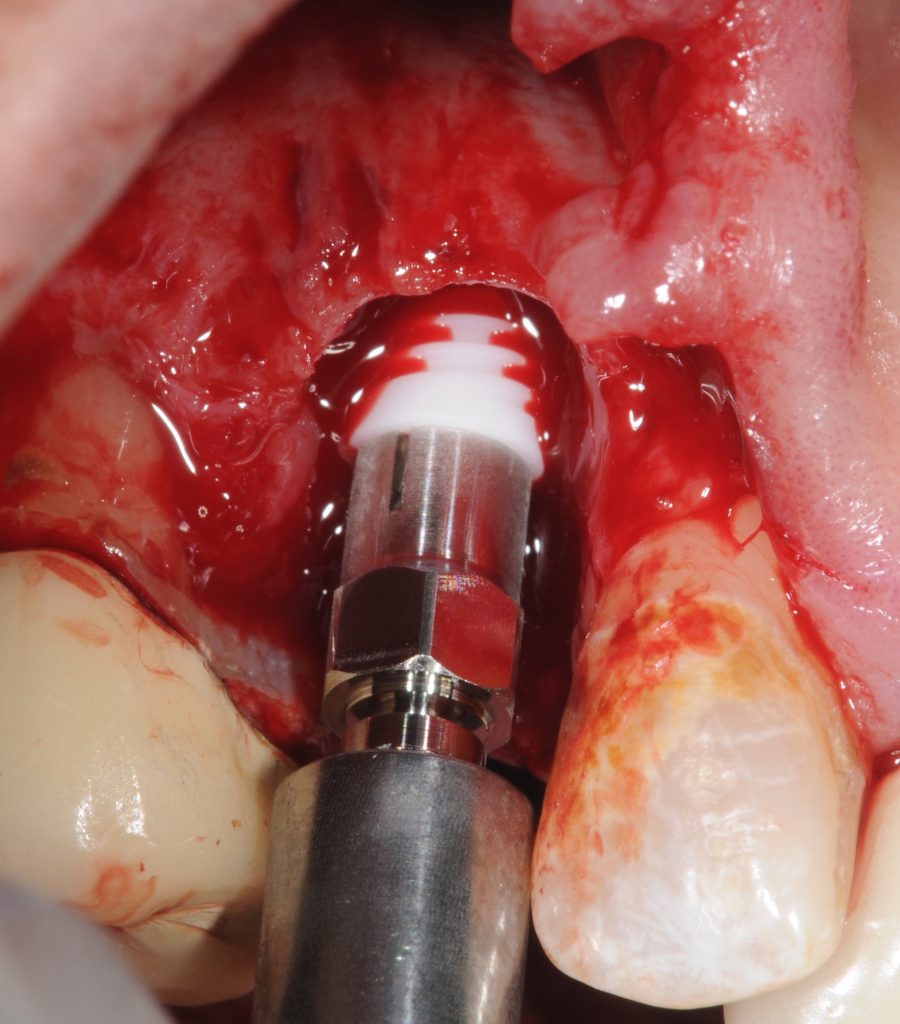
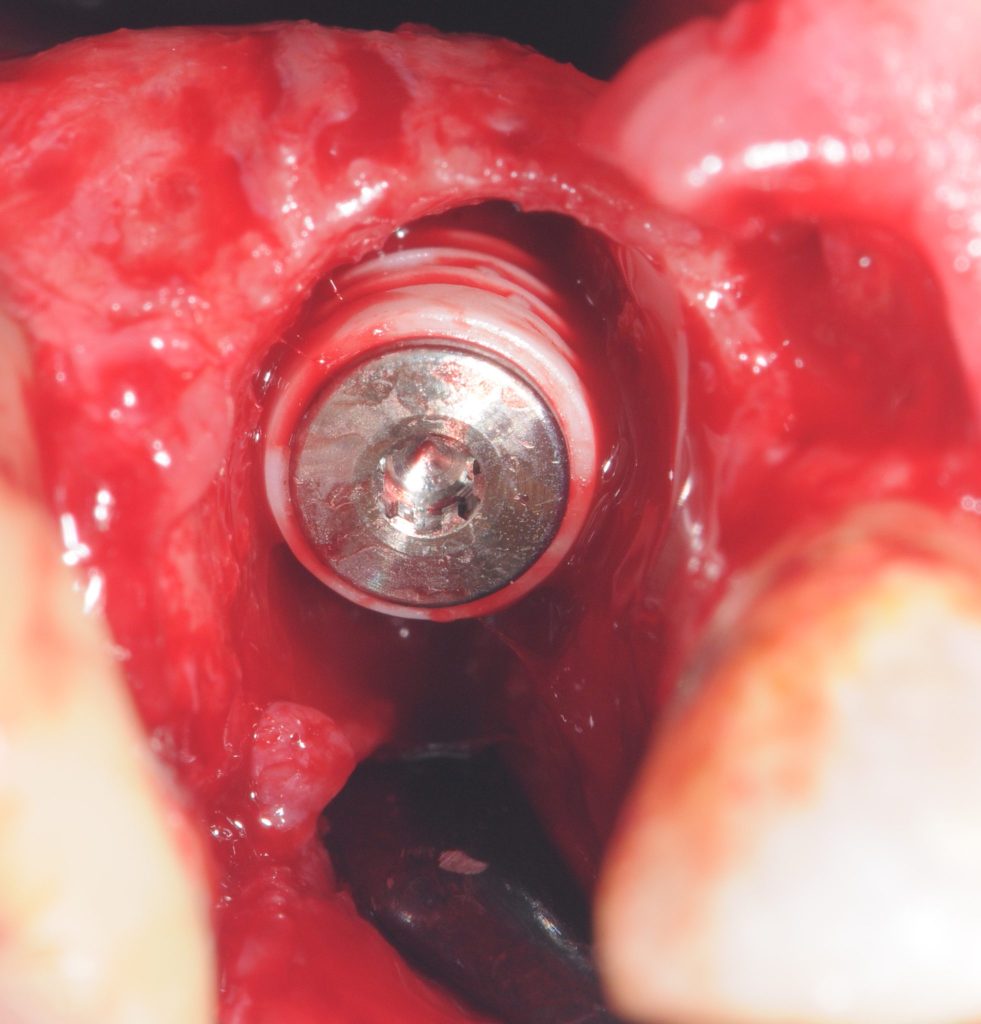
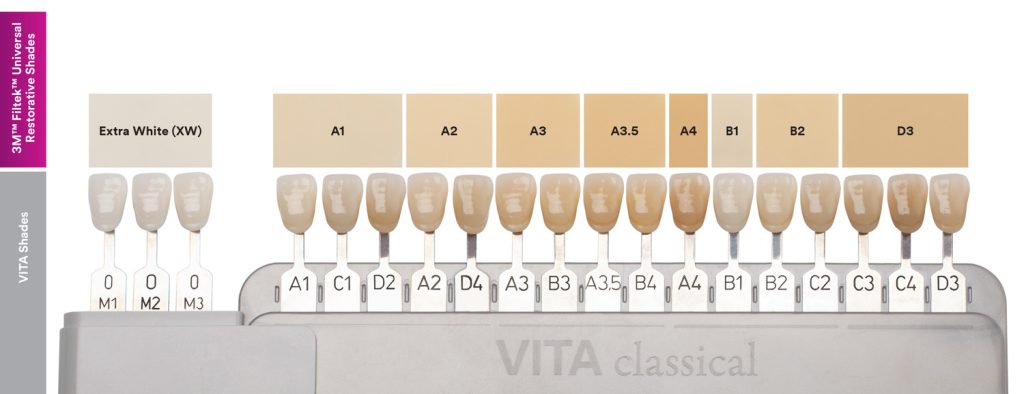
As such, one way to overcome these challenges is to find a product that has been clinically proven to mask stains. Filtek Universal Restorative from 3M is an excellent option. Its Pink Opaquer shade covers stains and eliminates dark areas,* meaning that you can then complete the restoration with your shade of choice for long-lasting, aesthetic results.
Prepared for all eventualities
Restorative dentistry brings a number of challenges, but stained dentition can be simple to overcome. By investing in products that can reliably mask any staining, you can feel confident that you are giving your patients the natural-looking results they require.
*3M internal data
For more information, call 08705 360036 or visit www.3m.co.uk/Dental
3M and Filtek are trademarks of the 3M Company.
[i] British Dental Association. Dental Amalgam. Link: https://bda.org/amalgam [Last accessed May 22].
[ii] Statista. Share of Adults With At Least One Tooth Filling in England 2018, By Region. Link: https://www.statista.com/statistics/1131889/adults-with-tooth-fillings-in-england-by-region/#:~:text=In%202018%2C%2090.2%20percent%20of,London%20have%20a%20tooth%20filling. [Last accessed May 22].
[iii] Healthline. How Tetracycline Affects Teeth and What To Do about it. Link: https://www.healthline.com/health/tetracycline-teeth [Last accessed May 22].




















 Your key to aesthetics
Your key to aesthetics

