Dr Nishan Dixit presents a case study with a 6-year follow-up where he took a minimally invasive approach to restore the function and aesthetic of his patient’s upper anterior teeth to an exceptionally high standard.
A 33-year-old female patient in good general health attended the practice complaining about the appearance of her upper anterior teeth. She was unhappy with the colour of the teeth and the fact that they were becoming thinner. She also reported that she did not smile as much due to the way that the upper central and lateral incisors protruded outwards. The patient had undergone two unsuccessful courses of orthodontic treatment in the past, so her goal was to have an improved smile with teeth that were aligned and all of a similar colour.
Assessment and diagnosis
A comprehensive dental health examination was completed and the patient’s oral hygiene found to be of a fair standard. The patient’s soft tissues, temporomandibular joints and masticatory muscles were also assessed, but this did not reveal anything abnormal. As there was nothing untoward with the patient’s existing occlusal scheme, it was decided that a conformative approach would be taken, utilising the existing maximum intercuspal position.
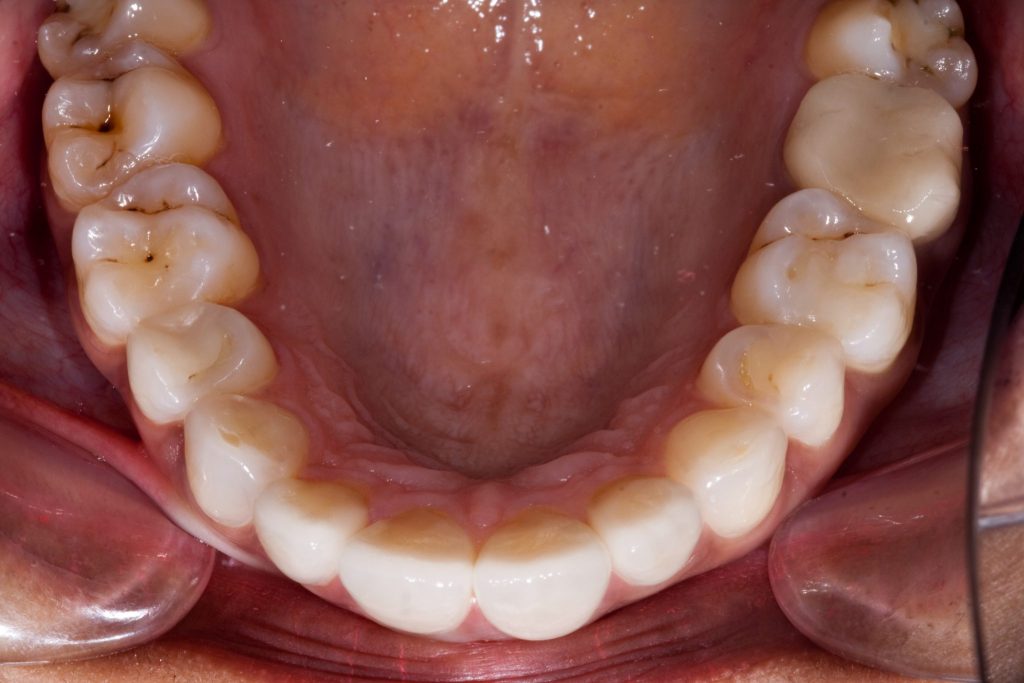
The loss of tooth substance was present on the palatal surfaces of the upper central and lateral incisors. The patient advised that she did not consume acidic beverages and had a limited intake of acidic fruits. She did not drink alcohol or smoke, but she did report having a funny, sour-like taste in her mouth upon waking up in the morning and even during the day sometimes. Therefore, it was diagnosed that the loss of tooth substance was due to regurgitated acid from gastro-oesophageal reflux.

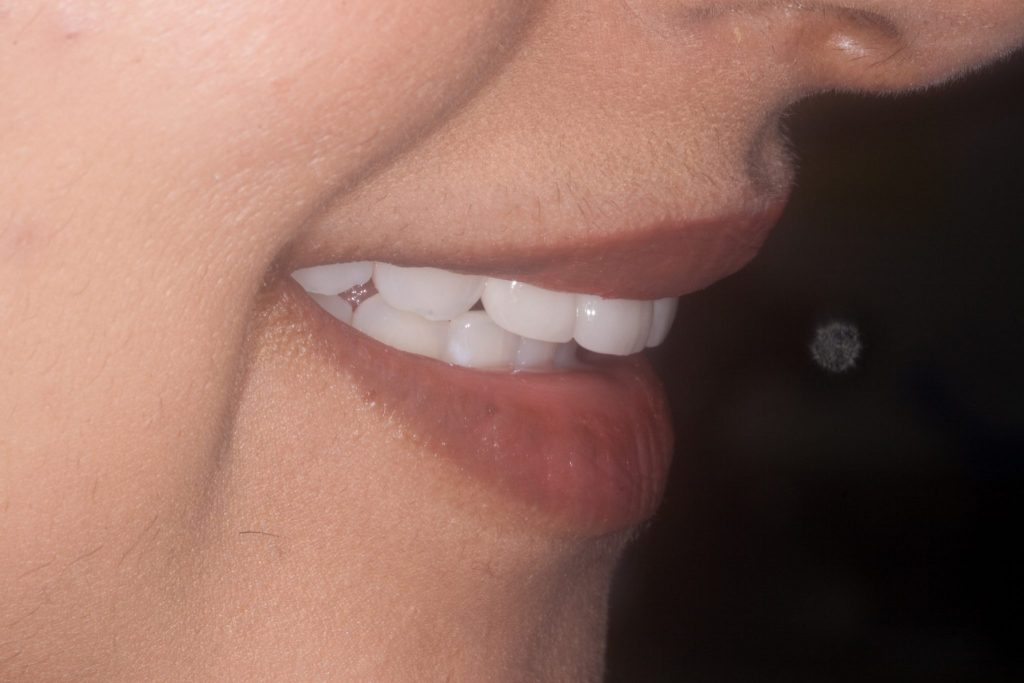
Figure 1 Initial presentation 
Figure 2 Retracted view of initial smile

Figure 3 Right side retracted view

Figure 4 Left side retracted view

Figure 5 Occlusal view of upper anterior teeth

Figure 6 Close up of upper central and lateral incisors
Treatment planning
The patient was instructed to see her general practitioner (GP) for advice and treatment regarding her gastro-oesophageal reflux diagnosis. The treatment plan was for the patient to undergo oral hygiene therapy with oral care and dietary advice provided. Professional tooth whitening treatment would then be performed with Philips Zoom! system, which would also involve the patient using the Philips NiteWhite tooth whitening kit at home for 3 to 4 days.
Following this, the patient’s carious teeth would then be restored with composite restorations. In addition, full coverage e.max dental crowns would be fitted to the upper central and lateral incisors once the patient had seen and approved a diagnostic wax-up. Upper and lower Essix retainers would also be worn by the patient during the night to maintain the arch form.
Restoration
The patient’s GP prescribed her some antacid medications to take on a daily basis. After a period of stability with her condition was achieved, we were able to proceed with dental treatment.
Initially, the patient’s bite was recorded using Futar D registration material from Optident Ltd. Study models and a facebow transfer were also recorded, enabling the case to be articulated onto a Denar articulator. Using this information, Ivan Knezevic – a dental technician from Woodlands Dental Laboratory – was able to create a wax diagnostic mock-up of the four proposed crowns for the upper central and lateral incisors. Alginate impressions were taken so that bleaching trays for the upper and lower arch could be made.
The first stage of treatment involved completing oral hygiene therapy on the patient. She then underwent professional tooth whitening treatment with the Philips Zoom! in-office kit, followed by 3 to 4 days of NiteWhite tooth whitening gel at home for one hour every day on the upper and lower arch. Once the new colour of the teeth had stabilised, the carious lesions on the patient’s posterior teeth were restored with composite enamel and dentine shades of Empress from Ivoclar Vivadent.
Once the patient had seen and approved of her diagnostic wax-up, treatment began with the e.max crowns. The upper central and lateral incisors were prepared with local anaesthetic. Preparation guides were used to ensure tooth reduction was minimal on the buccal and incisal aspects of the teeth. Very little preparation was required on the palatal aspect due to previous acid erosion, so the margins were simply redefined.
At this point, additional bite records were taken. An occlusal stick bite was also recorded to ensure that the horizontal plane of the new e.max crowns was level with the interpupillary line. The final impression was taken using Provil Novo putty and a medium bodied wash from Kulzer. Temporary gingival retraction was achieved by using KaVo’s Expasyl for approximately 2 to 3 minutes.
Following this, custom temporary crowns were made using DMG Luxatemp. These were produced from an initial pre-operative impression and modified with the DMG Luxaflow flowable composite. Once we were happy with the size and shape of the temporary crowns, they were glazed with DMG Luxatemp Blaze & Bond. The crowns were then cemented into place temporarily using Temp Bond Clear.
The patient was left to trial the temporary crowns – the height of the central incisor crowns was 11.5mm and the width 9mm. At the review stage of treatment, minor adjustments were made to the mesial line angles of both the UL1 and the UR1, and the incisal edges of these teeth also levelled.
Once the patient was happy with the length and shape of her proposed new teeth, another alginate impression of the upper arch was taken so that the dental technician would be able to replicate the dimensions of the temporary restorations when making the final e.max crowns. A shade was chosen with the aid of the Optident Ltd Trushade device and a Vita shade guide, following Vanini’s shade mapping technique. This involves using a chromatic chart and colour card to determine the colour of the restoration.[i]
After administering local anaesthetic to the area, the new e.max crowns were fitted using 3M RelyX cement. The crowns were etched and silanated prior to seating. The patient’s occlusion was checked in all excursions using Hanel occlusion foil 12mm and Shimshock. She returned to the practice 10 days later and did not report any complications or discomfort following treatment. She was very happy with the final result and could now smile with confidence. At this stage, Essix retainers for the upper and lower arch were produced and provided to the patient to wear on a nightly basis. She was advised that retention is for a lifetime.

Figure 7 Shade matching 
Figure 8 Posterior teeth restored with composite

Figure 9 Patient’s smile with temporary crowns
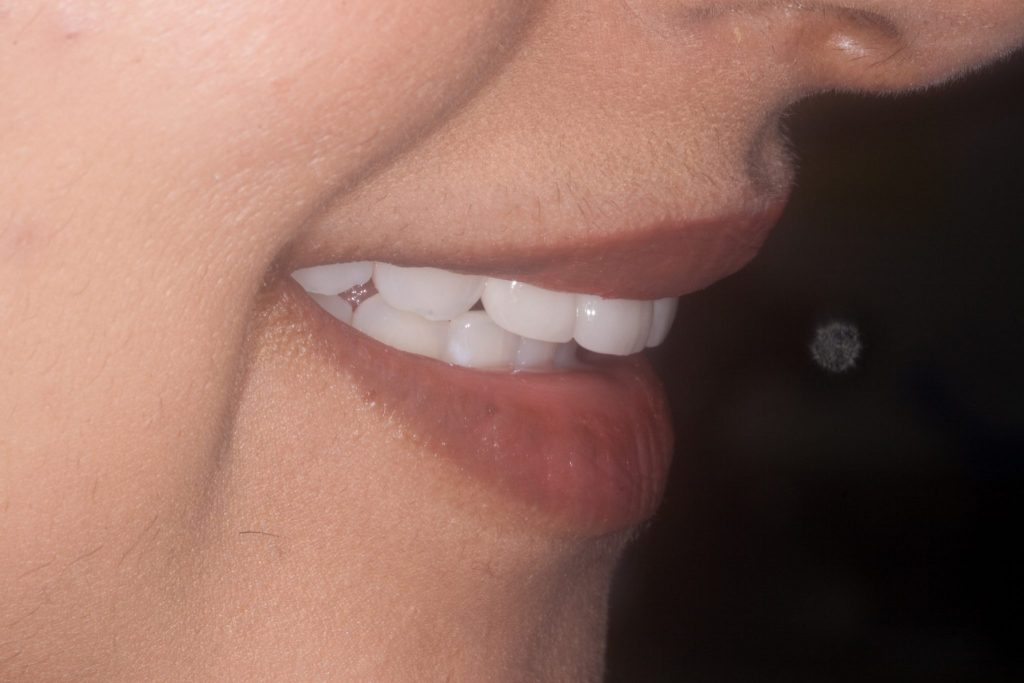
Figure 10 Right side view of smile with temporary crowns

Figure 11 Left side view of smile with temporary crowns

Figure 12 Retracted view of temporary crowns

Figure 13 Occlusal view of temporary crowns

Figure 14 Full view of patient’s face with final e.max crowns

Figure 15 Patient’s smile with final crowns

Figure 16 Right side of smile with final crowns

Figure 17 Left side of smile with final crowns

Figure 18 Retracted view of final crowns
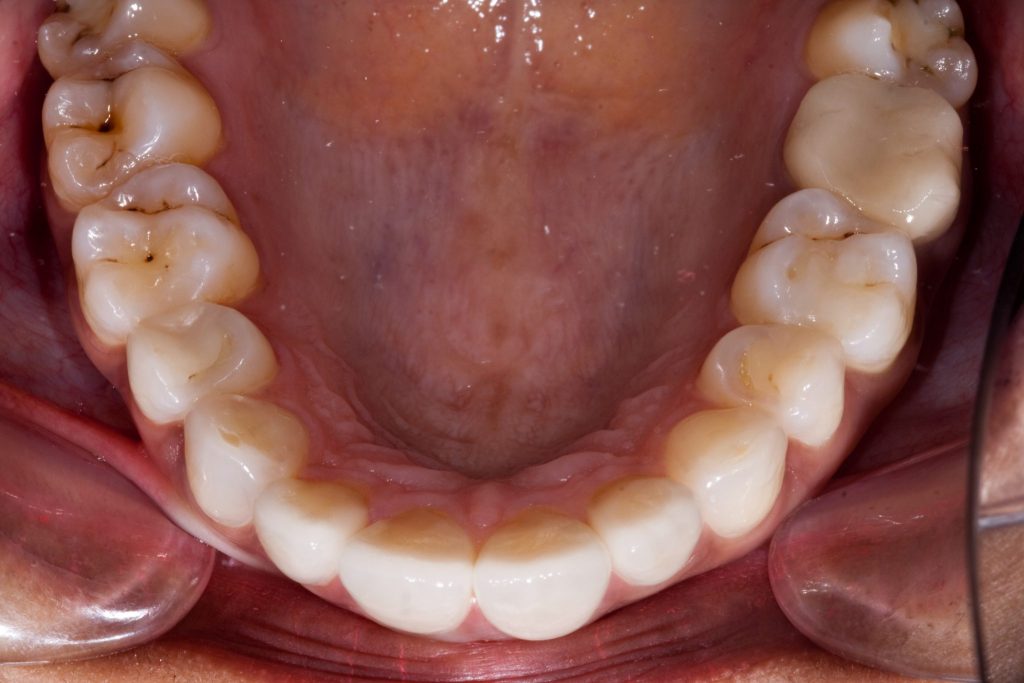
Figure 19 Occlusal view of restored upper anterior teeth

Figure 20 Close up of upper central and lateral incisors

Figure 21 Right side view of restored teeth

Figure 22 Left side view of restored teeth
Review and reflection
Figures 23, 24 and 25 demonstrate the stability of colour, gingival health and integrity of the e.max crowns after a 6-year follow-up of the patient. She remains highly motivated and continues to attend the practice every 3 to 4 months for oral hygiene appointments. She also wears her retainers on a nightly basis.
In this case, the patient’s aesthetic concerns were effectively addressed and the appearance of her smile improved with minimal tooth reduction. With the popularity of cosmetic dentistry continuing to rise, the need for conservative approaches to treatment is becoming much more apparent. This can be beneficial for both patients and practitioners, making treatment more comfortable and maximising the result to achieve optimal patient satisfaction.

Figure 23 Patient’s smile after a 6-year follow-up

Figure 24 Retracted view of smile after 6 years

Figure 25 Close-up of restored teeth after 6 years
For further enquiries about the British Academy of Cosmetic Dentistry, visit www.bacd.com
Author bio:
Dr Nishan Dixit qualified from Guy’s Dental Hospital in 1994. After qualifying, he worked as an associate in a couple of practices in northwest London for 5 years. In 2000, he established Blue Court Dental in Harrow, Middlesex. Being in a general practice environment, he covers all aspects of dentistry. However, he has a particular interest in minimally invasive aesthetic dentistry.
Dr Dixit is currently the President of the British Academy of Cosmetic Dentistry (BACD) and previously was the Scientific Director. Prior to this, he served on the Anglo-Asian Odontological Group (AOG) Committee for 10 years in various capacities. Following his passion has led him to be trained by leading clinicians both nationally and internationally.
[i] Vanini, L. and Mangani, F. M. (2001) Determination and Communication of Color Using the Five Color Dimensions of Teeth. Pract Proced Aesthet Dent. 13(1): 19-26.