The British Dental Association has warned that recent moves to ease the high levels of pandemic restrictions facing dental practices in England are unlikely to soften access problems, as new evidence from Healthwatch England highlights the ongoing crisis facing dental services, including the high numbers of children missing out on care.
According to a survey of high street dentists in England:
- Nearly a third of dentists (33%) have said they have no intention of relaxing COVID precautions, in line with new protocols issued by NHS England in November. Half say the arrival of the Omicron variant has had a high impact on their willingness to ease restrictions. Until the changes took effect, dentists have had to maintain gaps of up to an hour between most treatments, to reduce the risk of viral transmission, an approach that has radically reduced patient numbers.
- In light of wider winter pressures, and expected surge in other conditions like flu and the common cold 62% say the changes – which place patients on two pathways given risk of respiratory infection – will make little to no difference to the volumes of patients they can treat.
- Over 40% of dentists indicate they are now likely to change career or seek early retirement in the next 12 months given the current pressures on the service. Over half state they are likely to reduce their NHS commitment. 1 in 10 estimate their practices will close in the next 12 months.
- The Government’s handling of NHS dentistry is having a devastating impact on morale. 72% state the lack of clarity over the government’s controversial imposed activity targets – widely expected to increase on 1 January 2022 – is having a high impact on their morale. 70% say the same given uncertainty over the direction of pledged reforms to the service.
- Nearly 2/3 of practices (62%) estimate they are continuing to operate under 70% of their pre-COVID capacity.
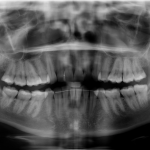
The BDA and Healthwatch both issue a joint message to Chancellor Rishi Sunak ahead of the budget to guarantee funding for the rebuild and recovery of services. At this time not a penny of the government’s multi-billion pound catch-up programme has been allocated to primary care dentistry. Over 37 million NHS appointments have been lost since lockdown in England alone, over 11 million for children. Tooth decay has been long established as the number one reason for hospital admissions among young children.
While the government has pledged reform of NHS dentistry by April 2022, the BDA has consistently warned that steps must be taken to stem the flow of talent from the workforce, and to provide the necessary resources to underpin any new system.
BDA Chair Eddie Crouch said: “It is tragic that so many million children are missing out on dental care. The government has a duty to ensure this does not become the new normal. For the sake of families across England we need to see real ambition from Ministers. Pandemic restrictions have been eased, but the gains appear modest at best. Patients are still struggling to secure appointments, and a frustrated workforce is looking for the exit.
“The Government keeps saying NHS dentistry is a top priority, but not a penny of investment has been offered. These problems are being felt in every community, and require deeds, not words.”