Original: 19:02, 06/02/2024
Latest Update: 09:10, 09/02/2024
NHS Dental Recovery Plan officially announced.
The British Dental Association has said government failure to embrace fundamental reform of NHS dentistry risks condemning a generation to decay and widening oral health inequality.
The professional body says the Recovery Plan, published today, is incapable of even beginning to honour Rishi Sunak’s promise to ‘restore’ NHS dentistry, or in any way meet the Government’s stated ambition to provide access to NHS dentistry for ‘all who need it’. The plan sets up a ‘new patient premium’, which will give a bonus to dentists seeing a patient that hasn’t undergone treatment in two years – £15 to first see them, £50 if they need significant work done. It also raises the minimum Unit of Dental Activity (UDA) value from the current level of £25.33 to £28.
The professional body had strenuously made the case for the Government to ensure dentists treating higher needs new patients that require more time in the chair, do not end up providing NHS care at a financial loss. It warns progress does not go anywhere near far enough to stop dentists – who operate as contractors not as NHS employees – being forced to cover costs out of their own pockets, particularly for treatments like dentures or crowns that require laboratory work.
There is no new money for this New Patient Premium, and so any new patients seen are just recycling the same limited pot of money. Factoring in late uplifts to contracts already promised by Government the BDA estimate fewer than 900 of the approximately 8000 NHS contract holders in England are likely to benefit from the higher UDA rate.
The £200m in ‘new’ money pledged is less than the half the underspends in the budget expected this year, the result of practices struggling to hit their punitive government targets. The BDA stress the ‘ring fence’ promised by Ministers to protect the dental budget remains an exercise in semantics, and that budget raids will remain the norm in cash-starved Integrated Care Boards.
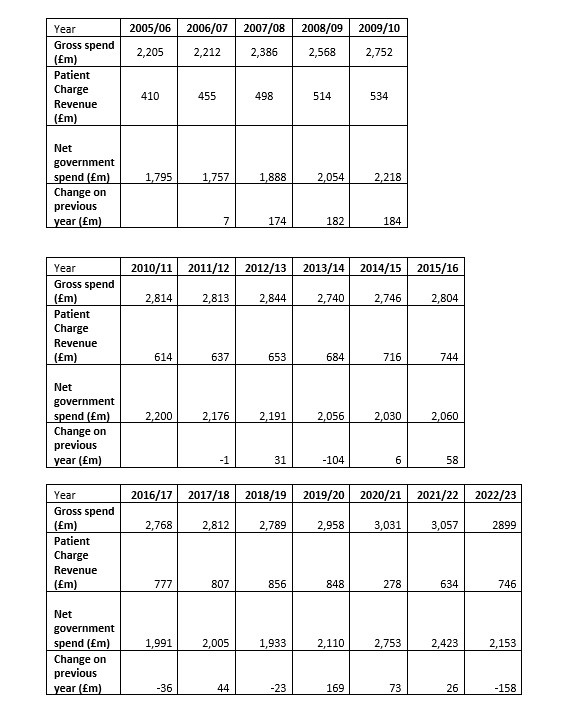
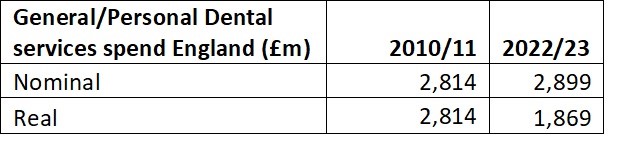
Any additional investment will barely begin to compensate for a decade of frozen budgets. Last month Department of Health and Social care accounts revealed the service’s £3bn budget has barely changed in a decade, with no effort to keep pace with demand, or rising costs. In real terms the budget has been cut by over £1bn since 2010.
The plan falls well short of the criteria set by the Health and Social Care Committee in its damning inquiry into dentistry. The BDA believes it singularly fails to honour MPs’ call for the “scope and ambition… to immediately address the crisis of access people across the country are experiencing.” The Government has ruled out reform of the discredited contract fuelling the exodus from the NHS. The Committee had stressed “fundamental reform of the dental contract is essential and must be urgently implemented, not only to address the crisis of access in the short-term, but to ensure a more sustainable, equitable and prevention-focussed system for the future.” In the absence of any meaningful change the BDA describe the package as amounting to little more than an exercise in ‘rearranging the deck chairs.’
With oral health inequality now widening the BDA has also said pledges merely to consult on preventive programmes like water fluoridation in the North East are close to meaningless, and that frontloaded investment in tried-and-tested schemes like supervised brushing are needed now.
The government is also reportedly going to offer dentists cash incentives to take on extra NHS patients, as well as sending teams to schools to treat children’s teeth. Under a plan to boost services in England, seen by the BBC, dentists will receive a “bonus” to take on more NHS patients, while up to 240 dentists will also be offered £20,000 to work for three years in under-served areas.
Police have recently had to break up crowds of hundreds attempting to get on the books with a new practice in Bristol. In the face of ongoing access problems new BDA surveys indicate 8 in 10 dentists have treated patients that have undertaken some form of ‘DIY’ dentistry since lockdown, amid reports of life-threatening dental sepsis surging, and British nationals even choosing to head to the Ukraine for care.
Leaks to the Daily Telegraph indicated that government was attempting to limit the political damage the crisis is doing in the coming General Election. The BDA stress the inadequacy of this plan will effectively ensure dentistry remains a major issue on the doorstep. From today the professional body will be working alongside the Daily Mirror and 38 Degrees to mobilise the public, to push for real change. https://38d.gs/SaveNHSDentistry
BSPD welcomes Government’s new dental recovery plan but flags absence of dental contract reform
in response to the Government’s dental recovery plan announcement, the British Society of Paediatric Dentistry welcomes the inclusion of measures to improve children’s oral health. This promise of funding and the implementation of measurable outcomes is pivotal to ensuring that at last the beleaguered NHS dental health services get the support needed to address the crisis in oral health in the UK today. However, the Society flags that there is an absence of a dental contract reform proposal to enable this.
Professor Claire Stevens CBE, BSPD Spokesperson, said: “This long-awaited plan includes some measures to tackle the crisis in children’s oral health. However, we cannot see a plan to review and revise the dental contract which is central to kick-starting the UK dental recovery. Is this the ‘elephant-in-the-room’? For too long we have had podium announcements which sound good, but are actually unworkable on the ground. We have been calling for clinically-informed policies with measurable outputs. The current dental contract is not fit for purpose and reform is long overdue.
“We need to ensure the funding is put to good use and supports the dental health workforce with a contract that works. In the run up to an election, we want to feel confident that these initiatives won’t just be shelved once the focus is off getting votes.”
Included in the plan are proposals to support water fluoridation, which BSPD has long supported as a proven intervention to improve oral health. There is mention of other initiatives such as the creation of mobile dental units. However, BSPD has some concerns regarding the value of mobile vans which include questions about a clear plan as to who will staff them, and secondly, requests reassurance that they will not just be for check-ups and fluoride varnish treatments, when the focus should be on targeting the most vulnerable children and rendering them dentally fit.
Professor Stevens added: “Our starting point if we could advise the Government would be to show them our 10 step Blueprint to dental recovery, which we sent to the secretary of health in November. We would want, as a minimum, the Government to commit to funding supervised toothbrushing schemes for the 20% most deprived children in England. This would be taking on board the valuable work done as part of the CORE20PLUS5 CYP initiative – which recognises that to make health care equitable, not just equal, some children will need more support to ensure that every child has the best start in life.
“BSPD supports the fluoridation of public water supplies in communities where the burden of dental decay is severe enough to warrant this public health measure and fluoridation is technically feasible. We look forward to seeing the details regarding the Government’s fluoridation plans.
“A preventively-focused dental services plan with funding and measurable outcomes is what we need. We look forward to seeing more details as the plans unfold and remain willing to work with all parties who commit to improving children’s oral health.”
College of General Dentistry issues ‘interim response’
The College has issued an interim response to the government’s press release announcing a ‘Dental Recovery Plan’, pending publication of the plan itself, which is expected later today.
Commenting on the proposals in the release, Dr Abhi Pal FCGDent, President of the College of General Dentistry, said:
“The government has today set out a range of initiatives intended to help tackle some of the many longstanding problems facing NHS dental provision in England. These include some potentially positive new initiatives, which we welcome, alongside previously made announcements. However, while some further positive changes to the dental contract are anticipated later this year, the Dental Recovery Plan does not represent the more fundamental contract reform which is required, nor will the additional £210m in funding behind the plan, welcome as it is, restore universal access to NHS dental care.
“We welcome the proposed Smile For Life programme, with its focus on intervening early to prevent oral diseases in children. Tooth decay remains the leading cause of hospital admission for 6–10-year-olds in England, and a preventative approach has the potential to reduce the need for restorative treatment. However, we wait to see whether sufficient resources will be invested for the programme to be a success.
“The additional temporary funding aimed at those who have been unable to access dental care for two years or more is much needed. However, we would like to see consideration of the ongoing care of individuals benefitting from this initiative.
“The intention to bring NHS dentistry back to some of the many communities who have lost access to it is also very welcome. While mobile units may help in the short term, bricks-and-mortar dental surgeries should remain the backbone of routine ongoing care delivery, and appropriate funding should be put in place to support the re-establishment of NHS practices to address lack of access and meet the volume of need.
“The planned ‘golden hello’ scheme brings implicit recognition of the difficulties experienced by dental practices in the recruitment and retention of clinical staff to deliver NHS dental care. However, we are concerned that this short-term offer may fail to overcome many practitioners’ long-term concerns about embarking on a career in NHS care delivery, among which are burnout, lack of career progression and insufficient recognition for enhanced skills.
“We are already looking forward to the expansion in the number of dental school places available for dentistry and dental hygiene students, and to the implementation of medicines exemptions for dental hygienists and therapists. Greater recognition and use of the full range of skills of all team members will enable the delivery of more care and make NHS dentistry more attractive to dental professionals. We also look forward to further proposals which empower the wider dental team when the next set of contractual changes are consulted upon.
“We also recognise that an increase in the minimum UDA value will support a small number of practices to continue delivering NHS dental care. And we support the intent to introduce community water fluoridation in areas of high need as this has the potential to reduce the prevalence of oral diseases and the need for invasive interventions.
“Finally, while dental practices struggle to recruit and many patients struggle to access care, there are many dental professionals who have qualified and practised overseas and who could be providing care here in the UK, but are unable to do so due to the waiting lists for the Overseas Registration Exams. So we welcome the possibility of provisional registration, and await the detail with interest.”
Denplan, part of Simplyhealth, issues response
Catherine Rutland, dentist and clinical director at Denplan, said: “The state of dentistry in Britain and scale of dental deserts has been a growing issue over the last few years. The initiatives suggested in today’s Dental Recovery Plan offer a glimpse of hope for the future – but only if introduced as part of wider policy changes.
“We can’t offer dentists more money for NHS patients while ignoring essential reforms to the dental contract so they can better treat the patients they have. The ability to offer a mixed NHS and private model would enable better support for both patients and professionals.
“Commitment to teach nursery pupils to avoid tooth decay is important to embed those early habits. However, we must also consider how we support parents with wider oral health habits, including dietary considerations, education and regular dental visits.
“This is a promising first step but more needs to be done – for our children, society, and our dental teams, many of whom are mentally and financially affected by the challenges facing the sector.”
Bas Vorsteveld, Haleon Vice President and General Manager Great Britain and Ireland, comments on behalf of Haleon
“Across the country we know that dentistry is under pressure and the this is having a major impact on the oral health of the nation. Latest figures show that 1 in 5 people have avoided visiting the dentist due to cost, more than double the same time last year. Today’s news of the UK Government’s Dental Recovery Plan marks an important moment in attempts to reverse that trend and build a more inclusive and accessible NHS dental service.
“At Haleon, we know that to truly tackle the major crises we face in the UK’s oral health we need to redouble our efforts on prevention. I’m pleased to see some steps in the Recovery Plan, such as the new ‘Smile for Life’ programme, which aims to tackle that. As a company we have extensive experience in this area, with our Aquafresh Shine Bright Academy, reaching kids in schools and showing them the benefits of better oral health. Focusing here is the way to sustainably improve oral health in the country and move pressure off oral health professionals.
“We also know that many oral health professionals are struggling to offer preventative advice due to short appointment times and lack of access to easy-to-share information. In fact, our recent Dental Health Barometer found that just one third of oral health professionals said they always offer preventative care advice to patients. With this in mind, the industry needs to work together to provide preventative care advice at different touch points – beyond the dental chair. This will ensure preventative advice is accessible to all and help encourage long-term oral health across the UK.
“We at Haleon are proud to continue to provide support and resources to dental health professionals in the UK. Although the impacts of the funding and initiatives may take some time to be felt, these are steps in the right direction with a long-term view. We are looking forward to seeing the roll out of the new Dental Health Recovery Plan and further steps needed to improve the oral health of the nation.”
Comment from the Oral Health Foundation
The Oral Health Foundation has broken down the key points of the plan to see if it’s really going to make a big difference, could be a good step forward, or should be dismissed as nothing but words on paper.
Dr Nigel Carter, chief executive of the Oral Health Foundation, says: “The new NHS dental recovery plan, while showing glimmers of hope with confirmed prevention policies like water fluoridation and expanded roles for the dental team, ultimately falls short of expectations.
“The heavy focus on childhood initiatives in underserved areas rather than addressing broader oral health disparities appears inconsistent and inadequate. It’s akin to applying an Elastoplast on a gaping wound.
“The recovery plan lacks the comprehensive, immediate solutions required to rescue NHS dentistry. The government’s vague response to a new dental contract is frustrating and deflating. This lacks any kind of detail or vision for the future of NHS dentistry, amounting to mere words. The absence of a commitment to scrap the unfair UDA payment system leaves patients and dentists in limbo. It feels like a postponement tactic, kicking the can down the road and passing the issue to the next administration without tangible progress.”
General Dental Council (GDC) welcomes the government’s positive response to improve international registration of dental professionals
The GDC welcomes the government’s commitment to improving the routes through which internationally qualified dental professionals can register to practise in the UK as part of their dental recovery plan.
The benefits of the legislative changes that the regulator encouraged the government to introduce last year are already being seen, with substantial increases in the capacity of the Overseas Registration Examination (ORE) already in place. But those legislative changes are still not fully in force, and it will take time to capture the full benefits, which starts with letting new contracts to providers. The procurement process for that is well underway.
The GDC is also pleased to see that the government has recognised the case they have been making for the introduction of provisional registration for internationally qualified dentists. This has the potential to bring dentists into the workforce more quickly, to help them adapt to practising in the UK environment with support and supervision, and to provide a valuable alternative to the ORE.
The regulator looks forward to working with the government to support the legislative changes necessary to create the provisional registration route – and to working with the health services and education providers of all four nations to develop the practical arrangements required.
As the government has acknowledged, exploring automatic recognition of international qualifications from outside the EEA is also a potential route to increase the number of dental professionals who can practise in the UK.
For all new dental professionals seeking to work in the UK, whether qualified here or in other countries, the GDC’s priorities are that standards are maintained, patients are safe, and the public are protected. Internationally qualified dental professionals make a vital and very welcome contribution to dental care across the UK, and the GDC wants to ensure that the registration process does not impose unnecessary obstacles. Increasing the flow of new international dental professionals can make a useful contribution to addressing the wider challenges of dental provision, but it cannot provide a solution to them.
Stefan Czerniawski, Executive Director, Strategy at the GDC, said: “We very much welcome the government’s openness to new ideas for ways of streamlining international registration. Provisional registration is an exciting opportunity that will require commitment and collaboration from across dentistry on the design and delivery of the new approach – we need to move at pace, but we need to take the time to get this right.
“We will not compromise on the standards we expect new registrants to meet, so we will need to work together to ensure that dentists will be effectively supervised and supported to practise while working under provisional registration, so that the public is protected.”
BADN welcomes plan as “a first step in the right direction”
The British Association of Dental Nurses (BADN), the UK’s professional association for dental nurses, has welcomed the Dental Recovery Plan as “a first step in the right direction” – but says the Plan “does not adequately address the current dental nursing recruitment and retention crisis”.
“The Recovery Plan is certainly a starting point,” said BADN Honorary President Joan Hatchard. “But it fails to take into account the fact that increasing the number of dentists/hygienists/therapists requires a similar increase in the number of dental nurses, as clinicians cannot work with dental nurses. The Plan blithely states that the NHS will also encourage more dental nurses to pursue training programmes – without giving any specific details on how this will be achieved!
“The recent survey carried out by Dr Debbie Reed of the University of Kent, in collaboration with BADN, shows that dental nurses are disillusioned by low salary levels (often only minimum wage), lack of career pathways, lack of recognition and support from their employers and are leaving the profession. The crisis in dental nurse recruitment and retention can only be resolved if these issues are addressed.
“BADN is happy to work with the appropriate organisations regarding implementation of the Plan, but urges those organisations to bear in mind that dentistry is not just dentists – dental nurses are the largest registrant group and the mainstay of the dental team. Dental nurses, and their needs, must be included in the equation!”