A newly published scientific review of findings from large-scale data research studies has examined the significant impact of diabetes and obesity on oral health and its potential role in preventing tooth loss. All the studies used real-world evidence gathered from large databases, some encompassing over 200,000+ individuals.
The joint review by the Department of Medicine, Shiga University of Medical Science in Japan and the Research and Development Department of Sunstar, owners of the oral health brand GUM®, specifically assessed the impact of diabetes and obesity on oral health with a focus on the number of remaining teeth. Most previous studies covered databases with fewer than 10,000 participants, limiting the ability for comprehensive analyses of remaining teeth. This review specifically focused on studies with large databases containing hundreds of thousands of study participants. They particularly focus in on two studies – co-initiated by Sunstar – that link dental visit records from insurance claims with health check-ups.
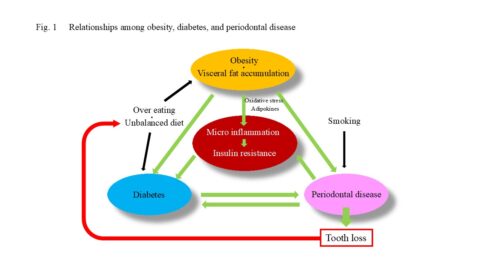
Previous studies also partially explained the relationship among diabetes, obesity, and periodontal disease. Adipocytes play a key role in energy storage and produce various adipocytokines. Visceral fat accumulation disrupts adipocytokine balance, inducing chronic inflammation and insulin resistance.
Diabetes and Periodontal Disease
The first study this review highlights is a recent meta-analysis of 15 cohort studies encompassing 427,620 participants. It confirms that individuals with periodontal disease have a significantly increased risk of developing diabetes, with a summary relative risk of 1.26. Conversely, 295,804 individuals with diabetes exhibited a 1.24-fold higher summary relative risk for developing periodontal disease relative to participants without diabetes – further implying a bidirectional relationship between periodontitis and diabetes.
One of the research group’s own studies analysed the association between the number of remaining teeth and glycemic control indices using a dataset of 230,000 individuals. The analysis revealed inverse relationships of glycated hemoglobin (HbA1c) and fasting blood glucose levels with the number of remaining teeth. This trend was evident even in individuals without a diabetes diagnosis (HbA1c levels of 5.5%–6.5% and fasting glucose levels of 110–126 mg/dL) and observed as early as people in their 30s.
The review further highlights a site-specific analysis of natural tooth retention, which showed that individuals in their 30s with HbA1c levels ≥ 7% were significantly more likely to lose posterior teeth than similarly aged individuals with HbA1c levels < 7%. For individuals in their 40s and over, this pattern extended to the loss of teeth adjacent to posterior teeth and anterior teeth. These findings suggest that poor glycemic control increases the likelihood of posterior tooth loss at a relatively young age, and that progression to more extensive tooth loss occurs with increasing age.
Combined Effect of Smoking on Periodontal Disease in Diabetes and Obesity
Besides diabetes, the authors also emphasize the association between obesity and tooth loss. One of their own studies showed how an increased BMI was associated with a decline in the number of remaining teeth. Compared to non-obese individuals (BMI < 25 kg/m²), those with obesity (BMI ≥ 25 kg/m²) had significantly fewer remaining teeth at 10 sites (six in the maxilla, four in the mandible) in their 30s, 19 sites (11 maxillary, eight mandibular) in their 40s, 24 sites (14 maxillary, 10 mandibular) in their 50s, and 21 sites (13 maxillary, eight mandibular) in their 60s.
But the associations between diabetes and obesity on the one hand, and periodontal disease and tooth loss on the other hand, may be influenced by other factors, such as smoking. In a previously published study by the same authors, highlighted in the review, analysis of 233,567 individuals revealed that nonsmokers with HbA1c ≥ 6.5% had a 1.83-fold increased risk of possessing fewer than 24 remaining teeth relative to nonsmokers with HbA1c < 6.5%. Among smokers with HbA1c ≥ 6.5%, the risk increased 3.55-fold compared with the same reference group, indicating the potentiating effect of smoking in patients with diabetes.
In an analysis of natural tooth retention according to site, the addition of smoking as a variable revealed an additional impact on tooth loss in locations unaffected by obesity alone. Further examination of the risk of possessing fewer than 24 remaining teeth showed a 1.47-fold increase in individuals with BMI ≥ 25 kg/m2 relative to those with BMI < 25 kg/m2.
The study’s authors note that the maintenance of good oral hygiene is a critical component of glycemic control in diabetic patients; effective glycemic control can help to prevent periodontal disease and tooth loss. This bidirectional relationship is also present among individuals with obesity and those with metabolic syndrome.
Recommendations of regular dental visits for patients with diabetes and obesity, as well as screening for diabetes and metabolic syndrome in patients with periodontal disease, may prove beneficial. Cessation of smoking, a well-established risk factor for tooth loss, can decrease this risk, with former smokers having no greater risk compared to nonsmokers.
This latest study highlights the bidirectional nature of obesity, diabetes, periodontal disease and oral health. Supported by previous reports, it emphasizes the importance of addressing the interconnected cycle of diabetes, obesity, and periodontal disease as a key strategy for healthcare and dental professionals to prevent tooth loss.
The full review can be accessed here in Current Oral Health Reports by Springer Nature.












