 Introduction
Introduction
The presence of a sufficient volume of bone is a key prerequisite of successful implant treatment. When working with deficient bone sites, clinicians must utilise additional techniques in order to facilitate implant stability and longevity. Ridge preservation is a proven bone grafting solution that can deliver enhanced implant success compared to other placement techniques[i] and can minimise the physiologic ridge reduction compared to extraction alone by up to 2.07mm.[ii]
For the best outcome for the patient, soft tissue changes must also be considered. The literature shows that autogenous soft tissue grafting and collagen alternatives are highly effective in maintaining or improving soft tissue volume alongside ridge preservation procedures.[iii] There is also evidence that an open wound healing approach leads to reduced gingival swelling and enhanced healing.[iv]
 The following case takes all of this into consideration and demonstrates the effectiveness of hard and soft tissue augmentation with a delayed implant protocol.
The following case takes all of this into consideration and demonstrates the effectiveness of hard and soft tissue augmentation with a delayed implant protocol.
The presenting situation
A female patient was referred for implant replacement of her failed upper right lateral incisor tooth. The tooth exhibited grade III mobility and had drifted forwards and downwards.
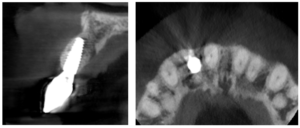
Clinical and CT scan assessment confirmed that the UR2 suffered from extensive bone loss with complete loss of the labial plate and was associated with a large periapical lesion which extended palatally and laterally towards the UR3. The UR3 tested positive to vitality testing.

 It was considered high risk to attempt an immediate implant placement in such a compromised site and the treatment plan was to firstly remove the tooth and the granulation tissue and perform a simultaneous ridge preservation procedure to combat the likelihood of severe shrinkage of the socket during the healing period. The rationale was to fill the bone defect with a bone graft material immediately after tooth removal to reduce the shrinkage of the socket and maintain most of the socket dimensions during the healing phase.
It was considered high risk to attempt an immediate implant placement in such a compromised site and the treatment plan was to firstly remove the tooth and the granulation tissue and perform a simultaneous ridge preservation procedure to combat the likelihood of severe shrinkage of the socket during the healing period. The rationale was to fill the bone defect with a bone graft material immediately after tooth removal to reduce the shrinkage of the socket and maintain most of the socket dimensions during the healing phase.
The ridge preservation procedure
The first treatment phase included the elevation of a large full thickness flap to fully expose the area and enable the harvesting of autogenous bone utilising a safescraper.

 The UR2 was then removed including excavation of all granulation tissue, taking care to avoid any direct curettage of the exposed UR3 root. The large bone defect was then filled with a 50/50 mix of autogenous bone chips and an allograft (MinerOss, a cortico-cancellous mix – BioHorizons Camlog) and the buccal defect was covered with a native porcine collagen membrane with a high percentage of collagen type III for a prolonged barrier function of six months. No fixation pins were used.
The UR2 was then removed including excavation of all granulation tissue, taking care to avoid any direct curettage of the exposed UR3 root. The large bone defect was then filled with a 50/50 mix of autogenous bone chips and an allograft (MinerOss, a cortico-cancellous mix – BioHorizons Camlog) and the buccal defect was covered with a native porcine collagen membrane with a high percentage of collagen type III for a prolonged barrier function of six months. No fixation pins were used.
The occlusal aspect of the bone graft – which would remain exposed during the healing period – was covered with a shorter acting native collagen membrane. The concept was that this exposed membrane would provide a barrier and prevent loss of the bone graft, but would also break down rapidly, favouring early epithelialisation of the open wound by secondary intention healing.

 The muco-periosteal flap was sutured back with 6.0 Prolene and no attempt was made to coronally advance the flap for complete closure. The rationale was to maintain the open socket wound and thereby preserve the original mucogingival relationship with no alteration. The socket entrance was sealed with the short acting membrane, while the original tooth (after root removal) was utilised as a temporary pontic and bonded to the adjacent teeth with flowable composite.
The muco-periosteal flap was sutured back with 6.0 Prolene and no attempt was made to coronally advance the flap for complete closure. The rationale was to maintain the open socket wound and thereby preserve the original mucogingival relationship with no alteration. The socket entrance was sealed with the short acting membrane, while the original tooth (after root removal) was utilised as a temporary pontic and bonded to the adjacent teeth with flowable composite.
Seven-month review
Healing was uneventful and following a seven-month maturation period, a CBCT scan confirmed the presence of the MinerOss/autogenous bone graft and a favourable volume of bone. However, it was noted that the soft tissues covering the bone graft were thin with an absence of interdental papillae. 
 It was determined that a connective tissue graft would be required as part of the next surgical procedure to improve the soft tissue volume and lead to the creation of papillae during the prosthetic stages.
It was determined that a connective tissue graft would be required as part of the next surgical procedure to improve the soft tissue volume and lead to the creation of papillae during the prosthetic stages.
Implant placement and soft tissue grafting
The second surgery involved a palatal crestal incision and a full thickness flap elevation revealing good turnover of bone graft into host bone. A bone level implant was placed in an appropriate three-dimensional position completely surrounded by new bone and no additional bone 
 grafting was required. A 4mm healing cap was placed.
grafting was required. A 4mm healing cap was placed.
A free gingival graft was taken from the palate below the upper right molar teeth and the epithelium was removed on the surgical table. The connective tissue strip of graft was then placed on top of the healing cap (and suspended over the healing cap) and secured to the palatal flap with 6.0 PGA Resorba Sutures. Finally, the buccal flap was closed with complete primary intention wound healing using 6.0 Prolene.
The provisional stages
 Three months later a small crestal incision was performed to expose and remove the healing cap and impressions taken to construct an under-contoured screw-retained provisional crown. Over a period of two visits, composite was incrementally added to the subgingival portion of the
Three months later a small crestal incision was performed to expose and remove the healing cap and impressions taken to construct an under-contoured screw-retained provisional crown. Over a period of two visits, composite was incrementally added to the subgingival portion of the

temporary crown to expand and modify the soft tissue emergence profile until an acceptable shape was achieved.
 A new impression was taken capturing the NEW transmucosal shape and a customised abutment and zirconia crown were fabricated as a one-piece screw-retained restoration and fitted to complete the case.
A new impression was taken capturing the NEW transmucosal shape and a customised abutment and zirconia crown were fabricated as a one-piece screw-retained restoration and fitted to complete the case.
 Three-year review
Three-year review
A three-year review of the final outcome displayed adequate hard and soft tissue volume with complete papilla infill and a pleasing outcome for the patient.
 Discussion
Discussion
This case study demonstrates the success of the open wound healing concept whereby the assimilation of a particulate bone graft was not impeded or compromised despite the fact that primary closure of the soft  tissues was not achieved.
tissues was not achieved.
It also highlights the importance of product selection for the bone augmentation procedure. I regularly choose MinerOss because the combination of cortical and cancellous particulate delivers fast yet controlled bone remodelling. Its rapid turnover to bone allows a shorter overall treatment time, creating a stable environment in which to place an implant only months after augmentation. I have also received excellent support from the team at BioHorizons Camlog for the approximately six years I have been working with them.





For product information from BioHorizons Camlog, please visit https://theimplanthub.com
Presented by Dr Robert Oretti
Dr Robert Oretti – BDS, MGDS RCS (LOND), MFDS RCS (LOND), MFDSRCPS (GLAS)
Robert qualified at Kings College, London in 1987. After working in an orthodontic practice in Colchester for four years he moved to Newbury, Berkshire. Rob then spent the next 14 years working in a busy private practice where he built a reputation for treating complex cases involving cosmetic, implant and orthodontic treatments. At this time, Rob also became involved in teaching and mentoring and has taught many dentists on all aspects of cosmetic and dental implant therapies. In 2006, Rob moved to Pentangle Dental Transformations – a purpose-built centre for dentists to send their patients for implant and complex treatments. Rob now spends his time between treating these referred patients and teaching. Rob is a post graduate tutor for the Thames valley deanery, a mentor and faculty educator for the ADI (Association of Dental Implantology), a mentor and international speaker for the ITI (International team of Implantologists), a Royal College of Surgeons examiner for the implant diploma (RCS Edin) and the Membership in Advanced General Dental Surgery (MAGDS RCS Edin) and was the president of BAAD (British Academy of Aesthetic Dentistry) 2018-2020. He presents regularly at scientific meetings and has published several articles on implant therapy.
[i] Yu X, Teng F, Zhao A, Wu Y, Yu D. EFFECTS OF POST-EXTRACTION ALVEOLAR RIDGE PRESERVATION VERSUS IMMEDIATE IMPLANT PLACEMENT: A SYSTEMATIC REVIEW AND META-ANALYSIS. J Evid Based Dent Pract. 2022 Sep;22(3):101734. doi: 10.1016/j.jebdp.2022.101734. Epub 2022 Apr 29. PMID: 36162892.
[ii] Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014 Oct;93(10):950-8. doi: 10.1177/0022034514541127. Epub 2014 Jun 25. PMID: 24966231; PMCID: PMC4293706.
[iii] Canullo L, Pesce P, Antonacci D, Ravidà A, Galli M, Khijmatgar S, Tommasato G, Sculean A, Del Fabbro M. Soft tissue dimensional changes after alveolar ridge preservation using different sealing materials: a systematic review and network meta-analysis. Clin Oral Investig. 2022 Jan;26(1):13-39. doi: 10.1007/s00784-021-04192-0. Epub 2021 Oct 20. PMID: 34669038; PMCID: PMC8791918.
[iv] Azab M, Ibrahim S, Li A, Khosravirad A, Carrasco-Labra A, Zeng L, Brignardello-Petersen R. Efficacy of secondary vs primary closure techniques for the prevention of postoperative complications after impacted mandibular third molar extractions: A systematic review update and meta-analysis. J Am Dent Assoc. 2022 Oct;153(10):943-956.e48. doi: 10.1016/j.adaj.2022.04.007. Epub 2022 Aug 25. PMID: 36030117.














 Introduction
Introduction  Three-year review
Three-year review Discussion
Discussion

