Dr Nick Fahey discusses an immediate implant case, which shows the difference that a digital workflow and guided approach can have for patient outcomes.
Introduction
Immediate implant placement guided by digital planning has been shown to deliver highly accurate results.[i] The literature also suggests that a guided approach to surgery affords time-saving benefits, as well as ensuring predictable and stable clinical outcomes, in addition to reduced post-operative discomfort for the patient.[ii]
To further enhance the clinical and aesthetic outcome in immediate implant cases, soft tissue management is often critical. When implemented appropriately, a connective tissue graft contributes to soft tissue stability alongside immediacy.[iii]
The following case demonstrates a combination of these techniques to deliver the very best result for a patient who had previously had a less-than-ideal implant experience.
Presentation
The patient was referred with a hopeless prognosis for the UL4. By the time they attended the practice, the crown of the tooth had completely fallen out and the tooth was fractured at the gingival level.
A full medical and dental history was taken, which revealed that she was taking HRT, had no allergies, was a non-smoker and didn’t drink alcohol. The patient was a regular attendee at her routine practice, where she had undergone clear aligner orthodontics in 2020. She also had existing implants in the UR6, UL5 and LL7 sites. Oral hygiene was good, reporting twice daily brushing and daily interdental cleaning. Her BPE score was 111/121 at the consultation.
The patient reported permanent numbness in the lower left-hand side of the lip after previous implant placements.


Treatment planning
The case was ideal for an immediate implant placement because the adjacent implant crown was less than ideal. It was important not to disturb the gingiva around this implant by raising a flap and the existing implant was also within very close proximity of the nearby molar. A minimally invasive approach was therefore indicated and an immediate workflow allows for this.
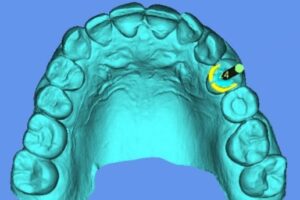
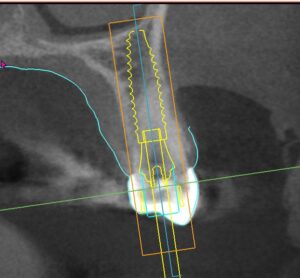
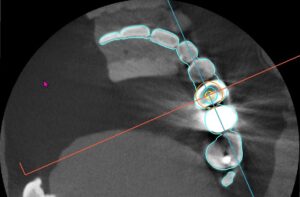
Using a digital and a prosthetically-driven approach, the ideal 3D implant position was determined. Guided surgery would be implemented in order to further ensure the least invasive procedure and optimise accuracy of implant placement given the narrow parameters being worked within. The necessary scans were used to fabricate the surgical guides and to transfer the planning to the surgical navigation software.
Hard and soft tissue augmentation would be required in order to ensure primary stability and enhance the long-term functional and aesthetic outcomes.




Surgical treatment
On the day of surgery, the UL4 was extracted atraumatically. The socket was thoroughly debrided and disinfected with a three-minute application of a chlorine dioxide gel. The socket epithelium was also removed with a diamond bur to prepare for the connective tissue graft (CTG).
Using both the static guide and surgical navigation, the osteotomy was performed. A slow drilling procedure <50 RPM was used to allow collection of autogenous bone, which was mixed with finely cut L-PRF membrane and PRF liquid to create a sticky bone graft material.
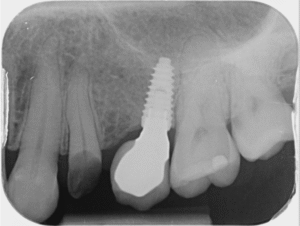
A 4.2mm x 15mm Tapered Pro Conical implant with Laser-lok was placed through the surgical guide and exactly according to the plan. The prepared autogenous mix grafting material was packed around the implant to fill any bony defects for increased stability.
A CTG was placed into a split-thickness pouch on the buccal aspect of the implant site, with some of the harvested soft tissue added to the de-epithelialised sulcus. The key here was to ensure that the graft material did not interfere with the neighbouring tooth to encourage papilla height and volume.
L-PRF membranes were placed over and around the implant site, with a laboratory-fabricated PMMA provisional crown added to stabilise the entire graft. This crown was left in situ for 12 weeks of healing.



Outcomes and reflections
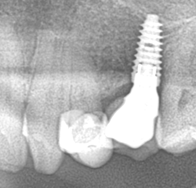
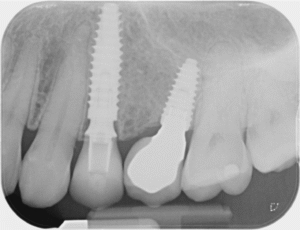
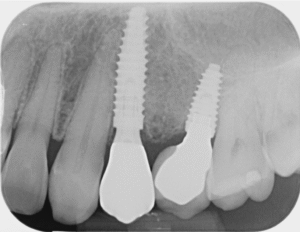
At the one-week review appointment the healing was uneventful. Radiographs were taken to confirm implant positioning and full seating of the provisional crown. After three months of healing, papilla height was maintained or improved, with the surgical site harmonious with the surrounding tissue colour, texture and volume for a very natural result.
Comparison of the UL4 implant with that in the UL5 provided in another clinic eloquently shows the difference that meticulous planning and execution can have on implant placement in a posterior region. Despite a potentially challenging situation, planning made the execution of treatment fairly routine. The ability to utilise immediate protocols also afforded the patient the many benefits associated with this type of treatment.




For more information on the Tapered Pro Conical https://www.biohorizons.com/Products/TaperedProConical.
Author Bio:
Dr Nick Fahey BDS, Mclin.Dent (Pros) MRD RCS(Ed), FRACDS and MFDS RCS (Eng.)
 Nick’s professional interests include all aspects of dentistry related to dental implants and fixed and removable prosthodontics. As a pioneer in computer-guided surgery, Nick has taught a generation of dentists about guided surgery and has been a KOL in this field for many companies. He is particularly interested in computer-guided surgery and guided surgical navigation for simplification of surgical placement of dental implants and has authored a textbook called “Guided Surgery. Making Implant Placement Simpler”. Nick is also a co-director of the FitzFahey Academy. Aside from his teaching and mentoring commitments, Nick works as a Specialist in Prosthodontics and is the Principal Dentist of Woodborough House Dental Practice in West Berkshire.
Nick’s professional interests include all aspects of dentistry related to dental implants and fixed and removable prosthodontics. As a pioneer in computer-guided surgery, Nick has taught a generation of dentists about guided surgery and has been a KOL in this field for many companies. He is particularly interested in computer-guided surgery and guided surgical navigation for simplification of surgical placement of dental implants and has authored a textbook called “Guided Surgery. Making Implant Placement Simpler”. Nick is also a co-director of the FitzFahey Academy. Aside from his teaching and mentoring commitments, Nick works as a Specialist in Prosthodontics and is the Principal Dentist of Woodborough House Dental Practice in West Berkshire.
[i] Xing Q, Lin J, Lyu M. The Accuracy of Immediate Implantation Guided by Digital Templates and Potential Influencing Factors: A Systematic Review. Int Dent J. 2025 Apr;75(2):439-452. doi: 10.1016/j.identj.2024.10.010. Epub 2024 Nov 8. PMID: 39521681; PMCID: PMC11976621.
[ii] Xiang B, Yu J, Lu J, Yan Z. COMPARISONS BETWEEN DIGITAL-GUIDED AND NONDIGITAL PROTOCOL IN IMPLANT PLANNING, PLACEMENT, AND RESTORATIONS: A SYSTEMATIC REVIEW AND META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS. J Evid Based Dent Pract. 2023 Dec;23(4):101919. doi: 10.1016/j.jebdp.2023.101919. Epub 2023 Aug 6. PMID: 38035896.
[iii] Seyssens L, De Lat L, Cosyn J. Immediate implant placement with or without connective tissue graft: A systematic review and meta-analysis. J Clin Periodontol. 2021 Feb;48(2):284-301. doi: 10.1111/jcpe.13397. Epub 2020 Nov 20. PMID: 33125754.
















