Dr Balaji presents a complex case in which sinus augmentation and hard tissue augmentation were required to replace a failing bridge with a multi-unit implant-retained prosthesis.
Patient presentation
A 70-year-old lady was referred to the practice for treatment of a failing four-unit bridge in the upper left region. The bridge was supported by UL3 and UL6 abutments, whilst the UL4 and UL5 were pontics.

Assessment and treatment planning
Initial assessment revealed the need to remove the existing bridge along with the UL3 and UL6. The patient had a thick gingival biotype, but there was severe bone and soft tissue loss at the treatment site, and the sinus floor was very close to the crestal bone in the region. A CBCT scan was taken at this stage.
Having taken all of this into account, the ideal treatment plan would include the extraction of the UL3 and UL6 and a delayed implant placement approach due to the significant bone and soft tissue loss. Hard tissue augmentation would be required in order to achieve optimal function and aesthetics, as well as maximise treatment longevity.
All treatment options were discussed with the patient, including the option of no treatment (which was not advised in this case). The patient provided informed consent to proceed with the above treatment plan, as this would provide good functional and aesthetic outcomes.
Treatment provision
The UL3 and UL6 were extracted and the site was allowed to heal for three months.
When the patient returned for the next stage of treatment, a crestal incision was made and a full thickness flap was raised. At this time, it was confirmed that there was buccal bone loss at the UL3 site and palatal bone loss at the UL6. Additionally, there was narrowing of the crestal bone in the UL4-5 region.

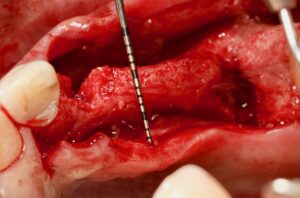
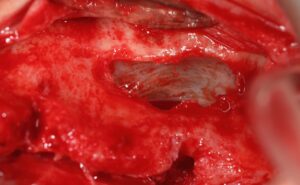
The sinus graft was harvested from the lateral wall and mixed with xenograft. A sinus graft procedure was performed with an external approach. A lateral window was created to access the sinus, the sinus membrane was lifted, and the graft material was placed. A guide was then placed for the implant stent to determine the prosthetically driven implant positions. Three dental implants were placed in the UL3,5 and 6 regions. The buccal defect was augmented using autogenous bone which was placed on the implant thread and layered with a mixture of xenograft and autogenous bone.





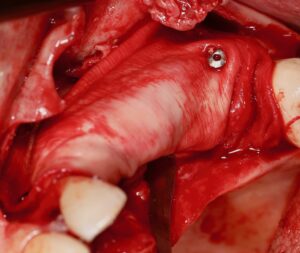
The grafting material was secured in place with a native collagen membrane using the sausage technique and stabilised with master pins. This technique aims to immobilise the bone graft and improve long-term stability. The flap was sutured for tension-free primary closure using the mucoperioelastic technique. After this stage of treatment was complete, the patient was provided with oral hygiene instructions to help keep the mouth clean during recovery, and help to ensure optimal healing.
After four months, the implants were exposed and the palacci technique was used to gain soft tissue thickness between the implants in the UL5-6 region. The palacci technique requires the careful manipulation of the peri-implant tissue to create soft tissue architecture similar to papillae.[i] This technique was successful and, after healing for two months, good gingival thickness was achieved in the area. The implants were restored with the final bridge.









Reflection
The biggest challenge in this case was the need to perform a sinus graft at the same time as bone augmentation. The patient was nervous about undergoing sinus and bone grafts. Fortunately, she had a thick soft tissue biotype, meaning that no extra soft tissue graft would be needed. The treatment provided resulted in a favourable outcome for the patient.
Dr Balaji provides industry-leading training courses on both hard and soft tissue management around dental implants with the ASHA Club.

For more information about how you could elevate your skills with the support of experts, please visit www.ashaclub.co.uk or call 07974 304269
Author bio:
 Dr Selvaraj Balaji: BDS, MFDS RCPS(Gla), MFD SRCS(Ed), LDS RCS(Eng)
Dr Selvaraj Balaji: BDS, MFDS RCPS(Gla), MFD SRCS(Ed), LDS RCS(Eng)
Since he obtained the BDS Degree, Dr Balaji has worked in Maxillo-facial units in the UK for several years and gained substantial experience in surgical dentistry. He is the principal dentist of The Gallery Dental Group which is made up of Meadow Walk Dental Practice and The Gallery Dental & Implant Centre. Dr Balaji is also the founder of the Academy of Soft and Hard Tissue Augmentation (ASHA) and runs courses, lectures and study clubs in the UK and around Europe for aspiring implantologists.
[i] Palacci, Patrick. “Papillae reconstruction: clinical considerations.” Faculty Dental Journal 3.1 (2012): 8-19.
















